
In the heart of Colorado’s Grand Valley, where the mesas meet the mountains, just "getting to the doctor" isn't always a simple ten-minute drive across town. For many residents in Mesa County and the surrounding stretches, a single medical appointment can represent a 100-mile round trip across stateline and over challenging terrain.
Enter Sunshine Rides of Colorado.
As one of the state's most innovative NEMT (Non-Emergency Medical Transportation) providers, Sunshine Rides isn't just moving passengers; they are bridging the gap between rural isolation and essential healthcare. Today, we’re sitting down with the team to see how they’ve scaled their "small-town" service into a regional powerhouse as they have expanded their fleet to cover more ground from Grand Junction to the San Luis Valley.
Sunshine Rides started with a single vehicle and a commitment to the community. With 35 years of experience serving Colorado, the company has evolved from a traditional taxi service into a specialized NEMT leader.
The challenge of rural transport is unique: low population density, unpredictable weather, and limited cellular reception in mountain passes. Sunshine Rides succeeded by leaning into these challenges rather than avoiding them. By specializing in Health First Colorado (Medicaid) transport, they’ve become the primary option for seniors and individuals with disabilities in areas where traditional public transit simply doesn't reach.
While many transportation providers stick to one lane, Sunshine Rides of Colorado has built a multi-faceted service model designed to solve the specific logistical headaches of the Mountain West. Here is how they are redefining what it means to be a "full-service" NEMT provider.
Most NEMT providers operate on a standard business-hour schedule, leaving patients stranded for late-night discharges or early-morning dialysis. Because Sunshine Rides maintains its roots as a professional car and van service, they are on the road 24 hours a day, 7 days a week in their headquartered city of Grand Junction and surrounding areas. Whether it’s a 3:00 AM hospital discharge or a weekend appointment, the "Sunshine" is always on.
In rural Colorado, a "local" specialist might still be three hours away in Denver or Salt Lake City. Sunshine Rides excels in long-distance medical transport. They don't just stay within city limits; their fleet is equipped and insured for statewide travel, regularly navigating the high passes to ensure patients in remote areas get to world-class facilities like the Anschutz Medical Campus.
Sunshine Rides is deeply integrated into the Home and Community Based Services (HCBS) program. This goes beyond a simple drop-off. It involves:
In an industry often bogged down by "hold music" and busy signals, Sunshine Rides offers a high-tech approach to booking. In addition to calling in a ride, passengers and caseworkers can schedule trips via:
The difference is Infrastructure vs. Intermediaries. Unlike national brokers who simply outsource rides to the lowest bidder, Sunshine Rides owns their fleet and employs their drivers.
They are locally owned and PUC-licensed, meaning they answer to the Colorado community, not a distant corporate board. When you call Sunshine, you're talking to someone who knows exactly where 28 Road is and understands how a sudden snow squall on I-70 will impact your trip. That local "ground truth" makes them untouchable in terms of reliability.
A provider is only as good as its last trip. For Sunshine Rides, the reviews reflect a deep-seated culture of care:
"We’ve used their competitors before, but Sunshine is in a league of their own. They are always on time, the drivers are friendly, and they treat my mother like their own family. In a place where it's hard to get help, they are a true blessing." > — Jeff U., Grand Junction
"As a wheelchair user, I’m often worried about the logistics of my appointments. Sunshine Rides makes it 'easy breezy.' Clear communication and professional drivers every single time." > — Andy M., Colorado Resident
Sunshine Rides of Colorado is the premier, locally owned Non-Emergency Medical Transportation (NEMT) and full-service car provider for Colorado's Western Slope. With a 35-year history of serving the community, they specialize in bridging the gap between rural residents and essential healthcare, operating a modern, fully-owned fleet equipped for wheelchair and bariatric needs. They are deeply integrated into the state's healthcare system, specializing in Health First Colorado (Medicaid SS) and HCBS Transportation.
Their commitment to the Mountain West extends beyond medical transport, offering a comprehensive suite of services including Taxi, Shuttle, Charter, Airport, Long-Distance, Event, and Sightseeing transportation.
Service Area Highlights
Contact & Accreditation
Accreditations
1. Does Sunshine Rides accept Health First Colorado (Medicaid)? Yes. Sunshine Rides is a premier provider for Health First Colorado members. Most Medicaid-eligible trips are covered at no cost to the member, provided they are scheduled through the appropriate broker or directly (depending on county regulations).
2. How far in advance should I book my ride in rural areas? In rural regions like Mesa or Montrose County, we recommend booking at least 48 to 72 hours in advance. This allows our dispatchers to optimize routes for long-distance travel and ensure a vehicle is available for your specific time.
3. Are vehicles equipped for wheelchairs and bariatric needs? Absolutely. Our modern fleet includes ADA-compliant vans equipped with hydraulic lifts and secure tie-down systems to ensure a safe, comfortable ride for passengers with mobility devices.
4. Does Sunshine Rides operate during winter weather? Our drivers are professionals experienced in Colorado mountain driving. While safety is our priority and extreme conditions may cause delays, we utilize advanced routing software to navigate around closures and keep our passengers on schedule whenever possible.

We’ve all been there: the phone rings, and a potential client asks for a non-emergency medical transport (NEMT) spanning several states. While these long-distance trips are high-value, they are often impossible for local providers to fulfill due to staffing, vehicle wear-and-tear, or licensing across state lines.
Usually, that’s a lost lead. But today, we’re changing the game.
We are thrilled to announce an exclusive opportunity for the Bambi community to monetize those "un-fillable" requests by referring them to our trusted partners at TransMedCare.
TransMedCare is a premier long-distance medical transportation specialist. They don’t compete with your local routes; they complement them. By partnering with them, you can turn a "no" into a professional "yes" while earning a significant commission for your business.
The beauty of this partnership is that it requires almost zero heavy lifting from your team. TransMedCare has streamlined the process so you can get back to managing your local fleet:
Because long-distance medical transport is a specialized service, the booking values are high. This isn't just "pocket change"—it’s a legitimate new revenue stream for your NEMT company.
Trip Type
Average Booking
Your 5% Commission
Minimum Trip
$5,000
$250
Average Trip
$8,000
$400
Imagine earning $400 just for spending one minute filling out a form for a trip you couldn't have taken anyway. It’s the ultimate win-win.
Stop letting those long-distance leads go to waste. Use your TransMedCare partner link today and start providing your clients with a total transport solution while boosting your bottom line.
SIGN UP TO BE A REFERRAL PARTNER: https://transmedcare-referral-partner.base44.app/?utm_source=bambi&utm_medium=referral&utm_campaign=partner_referral_program&utm_content=v1
Andrew Brainard, CEO of TransMedCare breaks down the long distance transportation process and how local NEMT providers can earn money as referral partners.

How a Virginia-based transportation provider is revolutionizing client-care through smarter technology
In the heart of Richmond, Virginia, MC MedRide has built its reputation on a simple but powerful promise: getting clients to their medical appointments safely, comfortably, and on time. But as anyone in the non-emergency medical transportation (NEMT) industry knows, delivering on that promise day after day requires more than good intentions—it demands operational excellence, precise coordination, and technology that works as hard as you do.
For MC MedRide, the path to becoming one of Richmond's most trusted NEMT providers meant finding a software solution that could match their commitment to customer care while streamlining the complex logistics of medical transportation.
Serving the greater Richmond metropolitan area, MC MedRide has distinguished itself through personalized service and unwavering reliability. Their team understands that for many clients , transportation isn't just about getting from point A to point B—it's about dignity, independence, and access to the healthcare they need.
Whether it's dialysis appointments that happen three times a week, routine check-ups for elderly patients, or specialized medical visits, MC MedRide has become a lifeline for clients and healthcare providers throughout the region. Their fleet handles everything from ambulatory transports to wheelchair-accessible vehicles, ensuring that every individual's unique needs are met.
Like many NEMT providers, MC MedRide faced mounting challenges as their business grew:
Scheduling Complexity: Coordinating dozens of daily trips across multiple vehicles while accounting for client-specific requirements, appointment times, and geographic efficiency required constant attention and adjustment.
Real-Time Communication: Keeping dispatchers, drivers, and patients informed about trip status, delays, or changes meant juggling multiple communication channels and constant phone calls.
Administrative Burden: Manual processes for billing, compliance documentation, and reporting consumed valuable hours that could be better spent on customer care.
Resource Optimization: Ensuring the right vehicle and driver were assigned to each trip while maximizing fleet utilization and minimizing empty miles was an ongoing puzzle.
These challenges aren't unique to MC MedRide—they're fundamental realities of the NEMT industry. But the right technology can transform these obstacles into opportunities.
When MC MedRide implemented Bambi's AI-powered NEMT software, they gained more than just a dispatch tool—they acquired a comprehensive operational command center designed specifically for the unique demands of non-emergency medical transportation.
Bambi's intelligent routing engine has transformed how MC MedRide plans their daily operations. The platform automatically optimizes routes based on real-time traffic conditions, client pickup windows, and appointment times, ensuring maximum efficiency without sacrificing service quality.
"The AI-driven scheduling in Bambi takes into account tasks we used to handle manually," notes the operational reality that many NEMT providers face. "Now our system automatically factors in wheelchair accessibility requirements, client preferences, and appointment durations to create schedules that actually work in the real world." Ingrid Redway, Owner
One of the most transformative aspects of Bambi for MC MedRide has been the dramatic improvement in communication and visibility. Dispatchers can monitor every vehicle in real-time, clients receive automated notifications about their driver's arrival, and healthcare facilities get confirmation when patients are picked up and dropped off.
This transparency has virtually eliminated the "Where's my ride?" phone calls that used to flood the dispatch center, freeing staff to focus on more complex coordination needs and customer service.
Bambi's comprehensive platform handles the entire trip lifecycle:
For MC MedRide, this integration means less time managing systems and more time managing customer relationships.
Perhaps the most significant impact of Bambi's platform has been enabling MC MedRide to refocus their energy on their core mission, exceptional customer care.
With administrative tasks automated and operations streamlined, drivers can spend more time assisting clients rather than completing paperwork. Dispatch staff can be proactive rather than reactive, anticipating needs instead of constantly managing crises . Management can analyze performance data and identify opportunities for improvement rather than being buried in spreadsheets.
The result is a virtuous cycle: better technology enables better service, which leads to happier clients, which builds stronger relationships with healthcare partners, which drives sustainable growth.
While MC MedRide measures success primarily through customer satisfaction and on-time performance, the operational improvements enabled by Bambi have been substantial:
These aren't just metrics—they're the foundation that allows MC MedRide to deliver on their promise to clients day after day.
As MC MedRide continues to expand their service area and fleet, they're doing so with confidence that their technology infrastructure can scale alongside their ambitions. Bambi's platform grows with them, handling increased trip volume without requiring proportional increases in administrative overhead.
The partnership between MC MedRide and Bambi exemplifies what's possible when NEMT providers embrace purpose-built technology that understands the unique challenges of non-emergency medical transportation. It's not about replacing the human element—it's about empowering people to do what they do best by removing the technological barriers that hold them back.
MC MedRide's story represents the future of non-emergency medical transportation: providers who leverage intelligent technology to deliver superior customer care while building sustainable, profitable businesses.
If you're facing similar challenges in your NEMT operation, complex scheduling demands, administrative burden, communication gaps, or growth limitations, Bambi's AI-powered platform can help you overcome them just as it has for MC MedRide and hundreds of other forward-thinking NEMT providers across the country.
Ready to see how Bambi can transform your NEMT operations? Schedule a personalized demo to discover how our platform can help you streamline operations, enhance patient care, and scale your business with confidence.
MC MedRide is a trusted NEMT provider serving the greater Richmond, Virginia metropolitan area. Committed to delivering safe, reliable, and compassionate transportation services, MC MedRide specializes in helping clients access the healthcare they need with dignity and comfort. Their fleet includes ambulatory and wheelchair-accessible vehicles equipped to handle a wide range of medical transportation needs, from routine appointments to specialized care visits.
With a focus on personalized service and operational excellence, MC MedRide has become a preferred partner for healthcare facilities, and clients throughout the Richmond region who demand dependable transportation they can count on.
Request a Ride with MC MedRide
Contact MC MedRide:
📍 Serving Richmond, VA and surrounding areas
🌐 Website: mcmedride.com
📞 Phone: (804) 845-0254
✉️ Email: admin@mcmedride.com

Managing a Non-Emergency Medical Transportation (NEMT) business involves handling drivers, vehicles, patient schedules, billing, and compliance. Dispatch software simplifies this by providing detailed reports that turn raw data into actionable insights. These reports help identify inefficiencies, track performance, and ensure compliance with Medicaid and broker requirements. Here's what you can expect:
These tools allow NEMT providers to improve efficiency, reduce costs, and meet regulatory standards, ensuring better service and smoother operations.

NEMT Dispatch Software Reporting Types and Key Metrics Overview
Trip performance reports provide a straightforward view of how your service is performing. They cover everything from pickups and drop-offs to cancellations and delays, helping you identify and address inefficiencies early on. These insights enable smarter decisions about scheduling and routing.
The data can reveal telling patterns. For instance, you might notice that certain routes are consistently delayed, or that specific drivers struggle with punctuality. Take the example of a California-based NEMT provider that serves patients with specialized needs. By adopting an integrated reporting system in 2025, they saw a 40% drop in late pickups. Such results show the power of actively monitoring and analyzing performance metrics.
Key metrics to review include on-time performance, trip completion rates, no-show rates, and ETA accuracy.
Two essential metrics to keep an eye on are on-time pickup rate and trip completion rate. The on-time pickup rate measures how often drivers arrive as scheduled, while the trip completion rate tracks the percentage of trips successfully carried out.
Using automated route optimization and reporting tools can improve on-time arrivals by as much as 50%. This not only enhances patient satisfaction but also reduces complaints and ensures more dependable service. For example, if you notice frequent cancellations at specific times or delays on certain routes, you can adjust pickup windows using historical data, reroute drivers to avoid traffic bottlenecks, and offer targeted training to drivers who need support.
In addition to punctuality, other metrics like no-shows and ETA accuracy provide valuable insights into your operations.
Tracking no-shows and ETA accuracy ensures a complete picture of your service. No-shows can be costly. When a patient misses a scheduled trip, resources like driver time, vehicle use, and fuel go to waste. No-show reports help identify patterns, such as patients who frequently miss appointments. By using smart dispatch systems and detailed reporting, you could reduce missed trips by up to 30% within three months.
ETA accuracy reports evaluate how reliable your estimated arrival times are. For example, if a patient is told their ride will arrive at 10:00 AM but it consistently shows up late, it damages trust in your service. A New York-based NEMT provider serving Medicaid patients tackled this issue by introducing real-time vehicle tracking and reporting in 2025. The result? A 60% drop in complaints about waiting times. Accurate ETAs not only improve patient trust but also make dispatch planning more efficient.
Driver activity reports offer a clear view of clock-in and clock-out times through mobile apps, using GPS to verify locations. This ensures accurate shift tracking and helps prevent time theft. The system also keeps tabs on critical credentials like driver’s licenses, CPR certifications, PASS training, and drug testing. Alerts notify you of upcoming expirations, so nothing slips through the cracks. Additionally, it categorizes staff as either W2 or 1099 employees, simplifying payroll and ensuring compliance with Medicaid and ADA requirements through timestamped records.
"NovusMED's reporting capabilities provides us the data we need to accurately invoice. The report integrates with our invoicing program – this has saved us a huge amount of time." - Cheryl Kastrenakes, Executive Director, Greater Mercer Transportation Management Association
Dispatch software generates detailed logs that include trip timestamps, odometer readings, and the number of patients transported during each shift. These logs are audit-ready and can be exported in formats required by major brokers, cutting down on administrative errors and speeding up reimbursement processes. For added convenience, you can integrate these logs with accounting tools like QuickBooks, making it easier to transition from activity records to invoicing and payroll.
Productivity reports go beyond basic record-keeping by evaluating driver efficiency and route performance. These reports measure key metrics such as trips per driver, deadhead miles (distance traveled without passengers), and route adherence using GPS data. This level of insight allows you to identify top-performing drivers and address inefficiencies. For example, if a driver accrues excessive deadhead miles, you can adjust their route or provide additional training.
Real-time dashboards allow you to monitor delays or conflicts as they happen, eliminating the need to wait for end-of-day reports. By reviewing weekly and monthly trends, you can forecast future performance and optimize staffing levels during peak demand periods. This proactive approach helps keep operations running smoothly while controlling costs.
After operational and driver reports, billing reports take financial management to the next level by ensuring accuracy and improving cash flow.
Modern dispatch software transforms trip data into billable claims, cutting out manual entry and reducing errors. These systems run automated checks for modifiers, payer rules, and coding issues before submission, increasing the chances of first-pass acceptance. Dashboards provide a clear view of claim progress, helping identify and resolve payment cycle delays and rejections.
In some cases, providers have implemented statewide claims systems in just 90 days, recovering thousands of dollars from previously lost submissions.
EDI claims tracking offers providers full visibility into each claim's status within the payment cycle. Advanced platforms integrate with top brokers like Modivcare and MTM, as well as state Medicaid portals, allowing providers to manage various submission formats and payer-specific rules from one system. GPS data is used to verify route accuracy, ensuring compliance and preventing penalties for overbilling or revenue loss from underbilling.
Denial management tools enable billing teams to quickly correct errors and resubmit claims. To reduce denials, link trip records directly to authorizations in the software, ensuring only approved rides are billed. This avoids issues like expired or missing authorizations. Additionally, comparing actual route geometry to pre-approved routes helps flag deviations so corrections can be made before claims are submitted.
This level of tracking also feeds into broader revenue analysis.
Invoice summaries, built on trip and driver data, reveal essential revenue trends. They classify revenue by payer type, enabling providers to see which contracts are driving the most activity. The software calculates revenue per trip, helping identify profitable routes and underperforming contracts. Aging Accounts Receivable (A/R) reports track how long invoices remain unpaid - sorted by payer type (e.g., Medicaid vs. private pay) - to pinpoint cash flow challenges.
| Metric | Target/Healthy Benchmark | Risk/Problem Zone |
|---|---|---|
| Clean Claim Rate | 95% or higher | Below 90% |
| Claim Denial Rate | Under 5% | Above 8% |
| A/R Days (Medicaid) | 30–45 Days | 60+ Days |
| Net Collection Rate | 95–99% | Below 95% |
| Write-Off Rate | Under 3–5% | Above 5% |
| First Pass Resolution | 85% or higher | Below 75% |
To maintain steady cash flow, weekly dashboard audits are recommended, as monthly reviews may miss fast-developing billing issues. Digital invoices can be generated and sent directly from the dispatch panel, streamlining the billing process and improving cash flow predictability. Providers can also download billing data to create summaries by provider, detailing claim counts and total amounts, which are useful for medical and contract audits.
Fleet and route reports go beyond billing to highlight inefficiencies and reveal cost-saving opportunities. These reports keep tabs on everything from fuel usage to vehicle idle time, offering actionable insights.
Automated route planning systems have proven to cut operational costs by 20%–30% and reduce fuel expenses by 15%–25%. By eliminating deadhead miles - achieving a 30% reduction through automation - fuel consumption drops, and driver utilization improves dramatically, jumping from below 60% to over 85%. This means more trips per driver, better deployment of specialty vehicles like wheelchair-accessible vans, and fewer vehicles left unused.
| Metric | Impact of Optimization/Reporting |
|---|---|
| Operational Costs | 20%–30% Reduction |
| Fuel Expenses | 15%–25% Reduction |
| Deadhead Miles | 30% Reduction |
| Driver Utilization | Increase from <60% to >85% |
Fuel reports provide a detailed breakdown of consumption by route, driver, and vehicle, helping to pinpoint inefficiencies. Dispatch software uses historical and real-time data to suggest the fastest, most fuel-efficient routes, steering clear of traffic jams and construction zones. Multi-load optimization reports also come into play, identifying chances to group compatible pickups into a single trip. This approach maximizes vehicle capacity while cutting down on total miles driven.
Utilization reports focus on balancing workloads across the fleet by monitoring idle time and usage patterns. GPS data can flag drivers with excessive idle times, which waste fuel unnecessarily. Reviewing productivity reports regularly can highlight low-density routes that might benefit from multi-load scheduling. Additionally, analyzing cost-per-trip data can identify specific vehicles or routes that are driving up expenses.
These insights not only boost efficiency but also pave the way for proactive maintenance and longer fleet performance.
Maintenance reports keep track of vehicle health, mileage, and repair history. They also trigger alerts for routine servicing, helping to avoid costly emergency breakdowns. Real-time odometer-based alerts, as opposed to fixed calendar schedules, ensure that service intervals are optimized, extending the lifespan of your fleet.
"The reporting software holds the capability of monitoring driver behaviour and vehicle maintenance. Transportation providers can use this feature to reduce the risk of accidents, and comply with safety regulations." - TripWizard
Route efficiency reports take fleet management a step further by refining scheduling and resource allocation using real-time data. These metrics ensure vehicles undergo regular inspections, maintaining compliance with safety standards. By reducing mileage and idle time, NEMT providers can significantly lower their carbon footprint while supporting broader community goals.
Detailed operational reports are great for managing the day-to-day, but centralized dashboards take things up a notch by providing a big-picture view. These dashboards blend compliance performance with business insights, offering a real-time snapshot of key metrics like Medicaid documentation and patient feedback. Modern dispatch software makes it easy to build customizable dashboards that bring everything together in one place. This saves managers from tedious manual data searches and ensures they have access to role-specific metrics tailored to broker contracts. By combining operational data - like trip performance and fleet reports - with compliance tracking and analytics, these dashboards deliver a unified, actionable view.
Just as driver logs and route data boost efficiency, compliance dashboards ensure providers are always audit-ready and following the rules. These tools automate the tracking of critical compliance elements, such as driver certifications, vehicle inspections, and trip documentation. They also use APIs to verify route accuracy and flag deviations that might lead to claim rejections or billing errors.
Take WellTrans, for example. In 2023, the company achieved full operational compliance in just 90 days by digitizing logs and trip details. This move created a clear audit trail for Medicaid, Medicare, and ADA reviews. On top of that, automated alerts for expiring credentials and upcoming inspections helped minimize the risk of compliance issues.
Meeting regulatory requirements is important, but custom analytics take reporting a step further by uncovering deeper operational insights. For instance, software can aggregate patient feedback and complaint data to highlight potential service issues. If a dashboard shows repeated delays on certain routes or with specific drivers, managers can address the root causes - whether that’s scheduling adjustments or additional training - before service quality takes a hit.
"Reporting in non-emergency medical transportation software can help identify patterns and trends in service delivery, enabling providers to make data‑driven decisions about resource allocation, route optimization, and driver training." – Momentm
Sure MET LLC is a great example of how custom analytics can transform operations. After switching to a specialized NEMT platform, the company recovered thousands of dollars in lost claims. The software flagged billing discrepancies their old system missed and revealed gaps in documentation and mileage tracking. By digging into cost-per-trip data and vehicle overhead, they pinpointed revenue leaks and fixed them.
Predictive analytics add even more value by forecasting high-demand periods, enabling providers to adjust staffing proactively. As brokers increasingly rely on data-driven scorecards to assign trip volumes, providers with clear and consistent metrics have a better shot at standing out in a competitive market.
Modern dispatch software helps you work smarter by turning operational data into actionable insights. This allows you to tackle inefficiencies, improve resource allocation, and make decisions grounded in facts rather than assumptions. By keeping track of key performance metrics, you can address problems swiftly and stay ahead of broker and regulatory expectations.
Automated compliance reporting simplifies staying audit-ready. It tracks crucial details like driver certifications, vehicle inspections, and trip documentation. Custom dashboards offer a clear view of revenue patterns and service gaps, giving you the tools to adapt and grow. Peter Drucker famously said, "If you can't measure it, you can't improve it", a sentiment that resonates deeply in NEMT. Transparent, reliable data fosters trust with brokers, healthcare providers, and patients, ensuring your operations run smoothly while meeting all necessary requirements.
Switching from manual vs. automated NEMT scheduling to automated reporting saves time, reduces errors, and delivers the transparency your stakeholders demand. Whether you're overseeing a small fleet or managing a large-scale network, these tools help you provide better service while keeping your business compliant and financially sound.
"The reporting tool equips providers with the knowledge they need to better their business every day." – Yurii Martynov, Marketing Director, RouteGenie
When it comes to Medicaid and broker audits, certain reports are critical. One of the most important is trip performance metrics, which include details like accurate trip documentation and route verification. These metrics ensure that every trip meets the required standards and can be verified.
Another essential component is billing and reimbursement summaries. These reports are crucial for confirming compliance with Medicaid reimbursement rules, helping to ensure that billing practices are accurate and align with regulatory requirements.
Together, these reports play a key role in showing transparency and maintaining adherence to the standards set by Medicaid and brokers.
Reporting helps cut down on late pickups and no-shows by providing real-time trip management, driver activity tracking, and performance metrics. With these tools, NEMT providers can make quick adjustments, enhance communication, and fine-tune scheduling. The result? Improved on-time performance and fewer missed appointments.
Billing reports play a crucial role in preventing claim denials. Reports that ensure accurate trip documentation - like trip performance and route verification reports - help confirm that all necessary details are properly recorded. Similarly, billing summaries that verify mileage accuracy and service details are key to minimizing mistakes that might result in claim rejections.

Non-Emergency Medical Transportation (NEMT) is undergoing a major transformation thanks to technology. Manual processes like spreadsheets and phone calls are being replaced by smarter, faster systems that improve efficiency, reduce costs, and ensure patients get to appointments on time. Here's how:
These tools not only save time and money but also improve patient care by reducing delays and missed appointments. As Medicaid and insurers demand better documentation, these systems provide audit-ready records and ensure compliance. For NEMT providers, adopting these technologies is key to staying competitive and delivering reliable service.
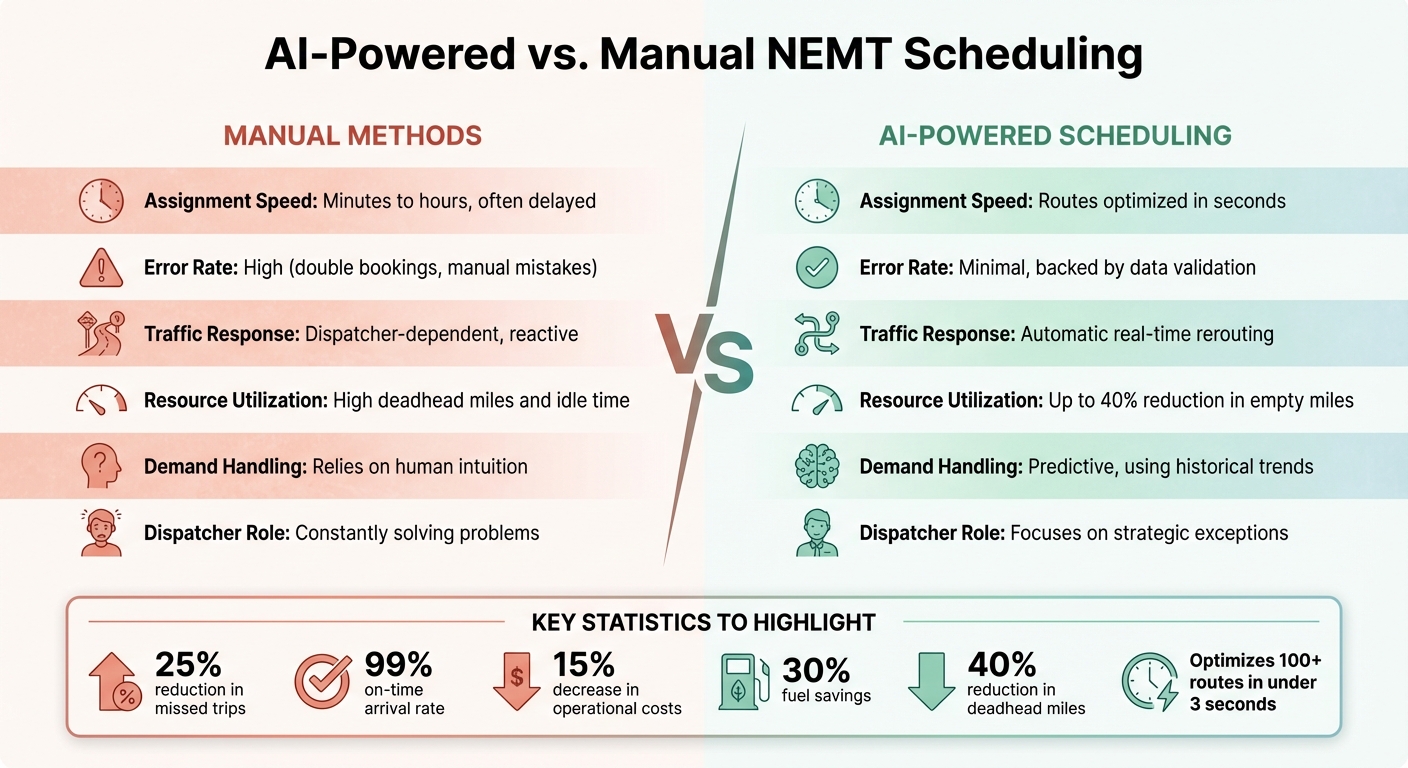
AI-Powered vs Manual NEMT Scheduling Comparison
AI-powered scheduling revolutionizes how Non-Emergency Medical Transportation (NEMT) providers assign trips. By analyzing real-time data - like driver locations, vehicle types, certifications, patient priorities, and traffic conditions - AI can match patients with the most suitable driver in just seconds. This automated process removes the guesswork and reduces human error that often plagues manual scheduling.
But it doesn’t stop at trip assignments. AI uses historical trip data, weather forecasts, and seasonal trends to predict demand patterns. This insight allows providers to prepare for peak periods by allocating more vehicles when necessary.
Recurring appointments also get a boost. AI systems embed patient preferences, such as specific pickup times and mobility needs, directly into daily schedules. This not only reduces administrative workload but also ensures a smoother, more reliable service experience for patients.
When disruptions occur - like accidents, road closures, or last-minute cancellations - AI steps in to adapt. It monitors live conditions and reroutes drivers automatically, reassigning trips in real time. In fact, it can optimize over 100 routes in under three seconds, saving dispatchers hours each day to focus on more critical tasks.
"The introduction of AI has revolutionized this process by transforming the dispatcher's role from a reactive problem-solver into a strategic manager." - NEMT Platform
The results of AI scheduling are both tangible and impressive. Providers have reported a 25% reduction in missed trips, a 99% on-time arrival rate, and a 15% decrease in operational costs. Fuel savings are significant too, with expenses dropping by up to 30% due to more efficient routing. Plus, “deadhead” miles - when vehicles travel empty - can be cut by 40%, which maximizes vehicle usage.
These operational improvements directly impact patient care. Reliable transportation increases treatment adherence by as much as 40%. For providers, financial perks go beyond fuel savings. AI systems automatically log trip details, mileage, and driver credentials, streamlining documentation for audits and insurance compliance.
AI also excels at handling complex scheduling constraints. It considers over 70 factors simultaneously, including vehicle capacity, driver hours, and specific patient needs like bariatric or standard wheelchair accommodations. This level of precision ensures compliance and maintains service quality, even as trip volumes grow.
Here’s how AI-powered scheduling stacks up against traditional, manual methods:
| Feature | Manual Methods | AI-Powered Scheduling |
|---|---|---|
| Assignment Speed | Minutes to hours, often delayed | Routes optimized in seconds |
| Error Rate | High (e.g., double bookings, manual mistakes) | Minimal, backed by data validation |
| Traffic Response | Dispatcher-dependent, reactive | Automatic real-time rerouting |
| Resource Utilization | High "deadhead" miles and idle time | Up to 40% reduction in empty miles |
| Demand Handling | Relies on human intuition | Predictive, using historical trends |
| Dispatcher Role | Constantly solving problems | Focuses on strategic exceptions |
Manual scheduling often forces dispatchers into a reactive role, constantly addressing issues as they arise. AI flips this dynamic by anticipating problems and resolving them automatically. For example, if a driver hits unexpected traffic, the system identifies and reassigns the trip to another available driver, ensuring the schedule stays intact.
Scalability is another major advantage. Expanding a manual system typically means hiring more staff, but AI can handle growing datasets and increasingly complex routing without additional labor costs. This scalability is vital as the NEMT market continues to grow, projected to reach $15.57 billion by 2028, with automation playing a key role in that expansion.
These advancements in scheduling pave the way for even greater improvements, especially when combined with real-time GPS tracking for fleet management.
Real-time GPS tracking works hand-in-hand with AI scheduling to give dispatchers a clear, instant view of their fleet. It shows exactly where each vehicle is, how fast it’s moving, and whether drivers are ready for new assignments. This level of visibility eliminates the guesswork of manual dispatching, which often relies on radio check-ins or phone calls.
When unexpected events like traffic jams, accidents, or road closures happen, GPS systems allow for immediate rerouting. This keeps schedules intact and helps avoid a domino effect of delays.
The benefits extend directly to patients. Instead of vague arrival windows, real-time GPS systems send precise ETAs via text or app notifications. Patients can even track their ride in real time, reducing stress and uncertainty. For instance, a New York provider serving Medicaid patients saw a 60% drop in complaints about wait times after adopting GPS tracking.
"Real-time GPS tracking also plays a big role, allowing dispatchers to monitor vehicle locations and quickly respond to any delays. This is crucial for patients who depend on timely transportation to attend medical appointments." - NEMT Platform
Modern GPS systems go beyond just showing dots on a map. They create detailed digital logs of trips, including routes, timestamps, and location histories. These records can be critical during audits or liability disputes.
Geofencing is another powerful tool. Dispatchers can set virtual boundaries around key locations - like hospitals or patient homes - and get automatic alerts when vehicles enter or leave these zones.
Driver behavior monitoring adds another layer of oversight. The system tracks risky actions like speeding, hard braking, and rapid acceleration. If unsafe driving is detected, dispatchers receive alerts and can intervene immediately. This not only improves safety but can also lower insurance costs and reduce wear and tear on vehicles. Additionally, if a vehicle breaks down or a driver faces an emergency, dispatchers can quickly reassign a nearby driver to ensure minimal disruptions.
These advancements directly improve patient care. Transportation delays cause nearly 30% of patients to miss appointments. Providers using real-time tracking have reported up to a 50% increase in on-time arrivals, which can lead to a 40% boost in treatment adherence.
Healthcare facilities also gain. Missed appointments due to transportation issues cost clinics about $200 per unused physician time slot. Live ETA sharing helps clinics better coordinate patient flow, reducing waiting room congestion.
Real-world examples highlight these benefits. A California provider saw late pickups drop by 40% after adopting GPS tracking. Meanwhile, a Texas-based provider saved over $50,000 in fuel costs in just six months while increasing monthly trip volume by 25%. They achieved this partly by cutting "deadhead miles" - the distance traveled without passengers - by up to 30%. Plus, while manual routing often results in driver utilization rates below 60%, GPS systems can push this number above 85%, enabling providers to serve more patients without adding vehicles.
These advancements lay the groundwork for even better results through NEMT route optimization.
While GPS tracking pinpoints vehicle locations, automated route optimization takes it a step further by charting the best routes. These AI-driven systems juggle multiple variables at once - like pickup points, appointment schedules, vehicle capacity, wheelchair accessibility, driver qualifications, and Medicaid's strict timing rules. They also integrate live traffic updates and weather conditions, instantly rerouting drivers to avoid delays and accidents.
Multi-stop planning is another game-changer. By grouping passengers into shared rides, the system minimizes "deadhead miles" - the distance vehicles travel without passengers. Instead of dispatching one vehicle per patient, the AI matches compatible passengers based on location and appointment timing. This strategy can cut deadhead miles by 30% to 40%. For instance, a Texas-based provider adopted this method in 2025 and saved more than $50,000 in fuel costs within six months, while also increasing trip volume by 25%.
AI also learns from past trends, like slower routes on Tuesday mornings, and adjusts schedules accordingly. This enables providers to achieve on-time pickup rates as high as 99%.
Route optimization can follow one of two paths: static or dynamic. Static routing relies on fixed schedules and spreadsheets, making it inflexible when unexpected changes arise. In contrast, dynamic routing uses AI to adapt in real time, recalculating routes within seconds when faced with last-minute cancellations or sudden traffic jams.
| Feature | Static Routing | Dynamic Routing (AI-Powered) |
|---|---|---|
| Input Factors | Manual data, fixed schedules, historical estimates | Real-time traffic, weather, GPS, and cancellations |
| Efficiency | Error-prone; struggles to scale with demand | Handles 100+ routes instantly; adjusts on-the-fly |
| Cost Outcomes | High fuel waste from backtracking and idling | 15-25% fuel savings; 30-40% fewer empty miles |
| Flexibility | Rigid; manual changes required | Auto-adjusts for no-shows and last-minute bookings |
This table highlights the advantages of AI-powered dynamic routing. A California provider experienced these benefits firsthand in 2025. By switching to AI-driven dispatch, they reduced late pickups and optimized routes based on predictive traffic data and driver availability. This eliminated the constant stress dispatchers faced when managing routes manually.
Adopting route optimization can slash fuel costs by 15% to 25%, and in some cases, up to 30%. These savings stem from cutting unnecessary miles, reducing idle time, and better grouping of trips. Operational costs drop by 20% to 30% overall.
AI systems also improve driver utilization, pushing it past 85%, compared to the under-60% efficiency typical of manual routing. This means providers can serve more patients without adding vehicles. Plus, fewer miles driven translates to reduced carbon emissions, aligning with community sustainability goals.
The benefits go beyond immediate savings. Optimized routing reduces vehicle wear and tear, extending the lifespan of the fleet and lowering maintenance costs. Combined with real-time GPS tracking and AI scheduling, automated route optimization creates a seamless system for maximizing fleet efficiency.
Modern communication platforms have become an essential addition to AI scheduling and GPS tracking and real-time monitoring, enabling instant and secure coordination between dispatchers and drivers. Unlike traditional radio and phone systems, which often cause delays and lack proper compliance records, these platforms combine VoIP, push notifications, and mobile driver apps into a single, unified dashboard. This eliminates the need for multiple tools and streamlines NEMT dispatch operations.
To ensure patient data remains secure, these systems use AES-256 encryption, meeting HIPAA standards for data protection during transmission. Role-based access ensures drivers only see the necessary trip details, such as pickup locations, mobility requirements, and appointment times. Additionally, all communications and transactions are logged, creating an audit-ready trail.
AI-powered virtual receptionists further enhance efficiency by handling routine inquiries 24/7. They can answer common questions like "Where is my ride?" and even book trips without human intervention, leading to a 40% reduction in call center workload for providers. Automated SMS and email reminders have proven effective in cutting no-show rates by 50%, while real-time ETA notifications keep patients updated.
Driver apps now support real-time, documented messaging, replacing outdated radio communication. Dispatchers can send updates about traffic delays, trip changes, or cancellations directly to drivers' smartphones, ensuring immediate delivery. Multi-channel systems, like those offered by Net2Phone, integrate phone, SMS, and email into one interface for seamless communication.
EHR and broker integrations are another critical feature, automatically pulling patient data from systems like Modivcare and MTM. This eliminates manual data entry errors and ensures that drivers have accurate information about mobility needs - whether a passenger requires a wheelchair, stretcher, oxygen support, or other assistance. Digital signatures and GPS-stamped events replace paper trip logs, reducing the risk of improper disposal violations and ensuring Medicaid audit compliance.
Automated alerts further improve coordination by notifying drivers, dispatchers, and patients simultaneously in the event of delays. For example, if a vehicle is stuck in traffic, the system recalculates the ETA and sends updates to everyone involved, all without requiring dispatcher input.
These advanced features improve both compliance and reliability. Encrypted communication reduces misunderstandings that could lead to missed pickups or address errors. For instance, Aerotranscare adopted an integrated platform to manage over 3,000 monthly trips, achieving a 98% on-time pickup rate while reducing call center volume by 40%. Similarly, Green Med Trans Inc. reached 88% automated dispatch coverage and a 99.2% claim approval rate for more than 5,000 monthly trips.
To protect patient data, these platforms enforce security measures such as automatic session timeouts and multi-factor authentication. If a driver leaves a device unattended, the app logs them out to prevent unauthorized access. Business Associate Agreements (BAAs) with software providers further ensure HIPAA compliance for handling Protected Health Information.
"One of my biggest issues before utilizing them was billing... In addition, the drivers love the app. It's user friendly and helps them to navigate around with ease!"
- Raquel Purvis, Owner, Goodwill Transportation Services
The shift to digital platforms has also significantly reduced paperwork and improved compliance. Helping Hands Transportation, for example, achieved an 80% reduction in paperwork and 100% compliance accuracy by transitioning from paper logs to a digital system. Considering that HIPAA violation fines can average $1.5 million, adopting secure communication tools is a critical investment for NEMT providers. These platforms not only enhance operational efficiency but also ensure seamless coordination and strict compliance across all aspects of NEMT services.
Non-Emergency Medical Transportation (NEMT) providers often grapple with issues like idle time, compliance audits, and unpredictable schedules. These challenges can directly affect both their service quality and profitability. However, advancements like AI-driven scheduling, GPS tracking, and modern communication tools are helping tackle these problems head-on. These solutions not only smooth out daily operations but also lead to noticeable improvements in efficiency and regulatory compliance.
Traditional scheduling methods often leave drivers underutilized. In contrast, AI-based scheduling tools can boost driver utilization rates to over 85% while cutting operational costs by 20% to 30%. These systems use real-time data - such as driver proximity, vehicle type, and certifications - to match trips more effectively.
AI also enables ride-sharing opportunities by grouping multiple passengers into a single trip. This ensures that vehicles are used more efficiently, reducing empty miles and fuel expenses. Considering that fuel and maintenance make up nearly 30% of operating costs, these savings can significantly enhance profitability.
Predictive scheduling takes it a step further by analyzing past trip data, weather conditions, and traffic patterns to anticipate demand surges. This allows providers to prepare schedules in advance instead of scrambling to handle last-minute requests. Additionally, dynamic route adjustments help drivers adapt to real-time changes like cancellations or traffic delays, keeping them productive. These optimizations can improve on-time arrivals by up to 50% and reduce travel times by 25%. Ultimately, these efficiency gains also help providers meet strict compliance standards.
Medicaid audits demand precise documentation, including pickup times, drop-off locations, and mileage. GPS tracking systems create a reliable, time-stamped digital record of every trip, offering geocoded proof that services were delivered as billed. States like Texas, New Jersey, and Florida now require GPS validation for reimbursement, making this technology indispensable.
Automated systems also reduce the risk of human error, which can lead to denied claims or costly clawbacks. Digital logs capture essential details like signatures, GPS data, and route maps, ensuring 100% accuracy during audits. These systems not only protect providers from fraud allegations but also comply with HIPAA regulations by encrypting sensitive patient information.
AI-powered fraud detection adds yet another layer of security by flagging irregularities in billing and trip data before claims are submitted. Predictive analytics further help providers avoid disruptions by monitoring vehicle sensor data and scheduling maintenance before breakdowns occur.
Recent advancements in technology are reshaping how Non-Emergency Medical Transportation (NEMT) providers operate. Tools like AI-powered scheduling, real-time GPS tracking, automated route planning, and modern communication systems are no longer optional - they’re essential for staying competitive and meeting compliance requirements. As Mindbowser aptly puts it:
"Technology is no longer an optional upgrade for NEMT operators. It has become the backbone of patient trust, regulatory compliance, and financial sustainability."
The numbers tell a compelling story: providers using these technologies report operational cost reductions of 20% to 30%, driver utilization rates above 85%, and on-time arrivals improving by up to 50%. Additionally, patient treatment adherence increases by as much as 40% .
The shift to digital-first operations is picking up speed. Medicaid brokers like ModivCare and MTM now demand rapid electronic updates and GPS-validated trips, with some states requiring GPS verification for reimbursement . Providers who stick to manual systems risk denied claims, lost revenue, and even contract disqualification. This is a critical issue as the global NEMT market is forecasted to grow from $8.65 billion in 2021 to $15.57 billion by 2028.
By adopting these technologies, NEMT providers can transform their dispatchers into proactive managers, ready to handle growing market demands while improving outcomes for patients, drivers, and business owners alike .
For those looking to start, focus on AI-powered scheduling and GPS tracking, then expand to automated route optimization and advanced communication tools. It's crucial to select systems that integrate seamlessly with billing and broker platforms to prevent data silos . The benefits are clear: midsize providers have reported saving over $50,000 in fuel costs within just six months, all while boosting service quality and ensuring long-term operational sustainability.
Switching to AI-powered scheduling can feel like a big step, but how challenging it is often depends on the systems you already use. The process usually involves a few key steps: migrating your existing data, training your team to use the new tools, and adjusting your workflows to fit the updated system. While the initial setup does take some effort, careful planning and support from your vendor can make the transition much smoother.
What makes it worth the effort? The benefits are hard to ignore. AI scheduling can boost efficiency, streamline routes, and enhance service reliability. For many providers, these advantages far outweigh the hurdles of getting started.
To meet Medicaid reimbursement and audit requirements, you'll need GPS-based proof that includes key elements like real-time tracking data, trip logs, and electronic proof of service. These records must confirm trip specifics, including timing and locations, in line with Medicaid transportation guidelines. Make sure your documentation is thorough and compliant to steer clear of potential issues during audits.
NEMT software works best when it seamlessly connects with billing and compliance reporting systems. This integration ensures accurate trip documentation and minimizes the chances of claims being denied - a common pain point in the industry.
For instance, tools like Post Trip Route APIs can simplify reporting processes. They help ensure that trips are properly documented while aligning with industry standards, making compliance much easier to manage.

Reliable transportation for patients with frequent medical appointments, like dialysis or therapy, is critical for their health and for NEMT (Non-Emergency Medical Transportation) providers' success. Manual processes often lead to inefficiencies, errors, and high costs, but AI-powered scheduling and route optimization tools are transforming how recurring trips are managed. Here's how to improve operations:
Comparing manual vs. automated NEMT scheduling shows how AI-powered software eliminates the hassle and errors of manual processes, especially for recurring patient transportation. Tasks like entering weekly dialysis or therapy trips no longer require hours of repetitive data input. Instead, dispatchers can create a trip once, and the system automatically repeats it - saving 2–4 hours per dispatcher each week.
Platforms like Bambi leverage machine learning to streamline scheduling. For example, its "Run Bambi Run" feature pairs passengers with the right drivers and vehicles, whether that’s a wheelchair-accessible van or a standard sedan for ambulatory patients. Julian Ssemalulu, Owner of Bellshan Homecare, shares how this has transformed his workflow:
"Bambi saves me about a whole days worth of time. Once I finished the dispatch I could go do other things and the system just does the work"
This software also simplifies bulk data management. Providers can upload up to 10,000 trip requests from brokers like Modivcare or SafeRide in one go, eliminating manual data entry errors. When last-minute changes arise, such as patient no-shows or added wait times, the AI dynamically adjusts schedules without disrupting the system. Let’s explore the core features and benefits of this approach for recurring patient trips.
The backbone of these platforms is their ability to automate standing orders. For instance, if a patient requires transportation every Monday, Wednesday, and Friday at 8:00 AM, the system schedules these trips indefinitely - until updates are made. It also factors in driver certifications and specific vehicle requirements, ensuring compliance with patient needs.
Constraint-based matching is another key feature. The AI assigns drivers and vehicles based on specific requirements like oxygen support or bariatric equipment. Automated notifications remind patients of their upcoming trips, reducing no-shows. Additionally, the system logs all changes to standing orders, maintaining an audit trail that supports compliance and troubleshooting.
These features result in major time savings. Booking a trip now takes just two or three minutes, cutting administrative time in half. Adham Harb, Operations Manager at CareTrips, highlights the broader impact:
"It's the easiest and best system that we have ever worked with scheduling wise... our trip count has gone up. Efficiency has gone up"
The software also eliminates common mistakes like double-booking drivers, forgetting holiday closures, or missing updates to treatment schedules. Jeffrey Hoff, Owner of Reliant Transport, underscores this:
"Switching over to Bambi is the most impactful thing I've done for my NEMT business. Bambi's AI is literally saving my staff hours of daily work"
Privacy is a top priority, with the platform maintaining HIPAA compliance during scheduling. With a 5.0-star rating across review platforms and recognition as the 2025 NEMTAC Innovation in NEMT Award winner, Bambi has earned its reputation for reliability. At $69 per vehicle per month, with no onboarding fees or long-term contracts, the software quickly offsets its cost by reducing administrative burdens and boosting trip capacity.

Manual vs AI-Powered Route Planning for NEMT Services
Efficient route planning plays a key role in ensuring patients reach critical treatments on time, especially for recurring trips. When trips happen regularly, consistency becomes non-negotiable - patients rely on dependable service week after week. Poor planning can lead to wasted fuel, frustrated passengers, and drivers stuck in preventable traffic jams.
Manual route planning often depends on a dispatcher’s memory and local know-how. While dispatchers might know common traffic patterns or details about destinations, this approach has its limits. Mistakes like double-bookings or missed road closures are common, and manual routes can’t adapt easily to changing traffic or conditions. On top of that, dispatchers typically spend an extra 2–4 hours each week managing these plans.
AI-powered systems, on the other hand, can analyze thousands of route options in seconds, accounting for real-time traffic, road closures, weather, and vehicle requirements. The results are impressive: on-time performance improves by 30% to 50%, fuel costs drop by 15% to 25%, and operational expenses are reduced by 20% to 30%. Driver utilization also jumps from under 60% with manual planning to over 85% when automation is used.
| Feature | Manual Route Planning | AI-Powered Route Planning |
|---|---|---|
| Planning Time | 2–4 hours per week per dispatcher | Automation reduces planning time by about 40% |
| Reliability | Prone to double-bookings and missed closures | 99% on-time performance; adjusts for holidays automatically |
| Fuel Efficiency | Significant fuel waste from "deadhead miles" | 15–25% fuel savings; 30% fewer empty miles |
| Adaptability | Struggles with real-time traffic or cancellations | Dynamic re-routing based on live conditions |
| Scalability | Limited by dispatcher hours and manual input | Supports 25–34% more trips without extra staff |
By incorporating detailed historical data, these systems can further refine route accuracy and efficiency.
Historical trip data can uncover patterns that manual planning might overlook. For example, analyzing six months of trip records helped one provider cut late pickups by 40%, while another reduced customer complaints about wait times by 60%.
Centralizing trip data - like pickup locations, times, mobility needs, and vehicle types - into a single digital platform is essential. Algorithms can then pinpoint recurring issues, such as specific patients missing appointments, consistently late routes, or clinics with long wait times. A Texas provider saved over $50,000 in fuel costs in just six months by using this data to eliminate unnecessary detours and streamline multi-stop routes. This also allowed them to increase their monthly trip volume by 25% through better vehicle use.
Smart systems can compare planned routes with actual outcomes, learning to predict arrival times more accurately over time. They also identify no-show patterns, allowing adjustments to schedules before dispatching drivers to pickups that won’t happen. For recurring trips, this means locking in routes that are both efficient and reliable, while still being flexible enough to handle last-minute changes without disrupting the entire schedule.
Clear communication is the backbone of smooth operations for recurring trips. When dispatchers, drivers, and patients are on the same page and can exchange updates quickly, everything runs more predictably. On the flip side, unclear protocols can turn minor delays into missed appointments and wasted resources. By combining automated notifications with real-time communication tools for drivers, operations can stay on track, even when unexpected issues arise.
Automated reminders play a key role in ensuring patients are prepared and reducing no-shows. Notifications sent via SMS or phone calls typically include essential details like the pickup time, driver’s name, and vehicle information. For recurring trips - such as those for dialysis or physical therapy, often referred to as "standing orders" - these reminders are especially important for maintaining access to critical treatments.
Two-way messaging adds another layer of convenience, allowing passengers to notify dispatchers about delays or ask questions. At the same time, dispatchers can send real-time updates about driver arrival times. Additionally, automated trip confirmations shared with healthcare providers improve reliability and help cut down on missed appointments.
While automated notifications keep patients informed, real-time communication with drivers ensures everyone stays in sync. Driver apps enable instant updates, helping teams quickly adapt to changes like traffic jams, cancellations, or last-minute adjustments. This is particularly crucial for return trips, where clinic discharge times can be unpredictable. Effective coordination in these moments minimizes driver wait times and keeps schedules on track.
Lisa M. from Metro Medical Transport highlights the importance of these tools:
"NEMT Platform has simplified my dispatching process and allowed me to focus on growing my business".
Drivers handling recurring trips play a key role in providing efficient, empathetic service, becoming a familiar and trusted part of a patient’s care journey. For individuals with regular appointments, such as those for dialysis or physical therapy, having a consistent driver can bring a sense of comfort and reliability. This specialized NEMT driver training aligns with operational goals, complementing AI-driven scheduling and route optimization.
Assigning the same driver to recurring routes helps transform transportation into a more personalized and supportive experience. Small gestures, like remembering a patient’s preferred vehicle temperature or accounting for extra time to assist with mobility aids, can make a significant difference in their comfort. NEMT software can store these preferences, allowing drivers to access them easily for every trip. As Ride with Excel Transportation explains:
"Every time we pick up a patient, we're not just providing a ride – we're becoming part of their healthcare support system."
Training should emphasize compassionate communication, teaching drivers to greet patients warmly, speak clearly, and actively listen to their concerns. A professional appearance and verified credentials also help build trust. Beyond improving patient comfort, a well-prepared driver contributes to smoother scheduling and more efficient routes.
While building rapport is essential, drivers also need to prioritize efficiency. Time management is vital, as delays can lead to missed treatments. Drivers should understand the importance of standing orders - recurring schedules many patients depend on - and recognize that missing treatments, like a dialysis session, can have serious health implications. Training should stress the importance of arriving 5–10 minutes early and using tracking apps to provide accurate updates. Drivers should also note patterns in patient readiness and confirm clinic schedules ahead of time, ensuring recurring routes run smoothly.
Even the most carefully planned recurring routes can hit snags - think extended appointments, vehicle breakdowns, or unexpected clinic discharges. That’s where real-time dispatch systems step in, dynamically tweaking routes and reassigning trips as needed. As Tobi Cloud puts it:
"NEMT scheduling software executes the plan; the real-time layer ensures the plan survives contact with real-world variability."
By building on AI-powered scheduling and dispatching, these systems ensure disruptions are addressed quickly. Using live GPS data, traffic updates, and constant monitoring, they help keep operations on track when plans go sideways. Instead of overwhelming dispatchers with constant updates, the software flags only the trips that need attention. This approach - called managing by exception - makes the process far more efficient.
Real-time systems shine when last-minute changes pop up, like a patient’s delayed appointment or an urgent new request. They can re-optimize routes instantly, removing completed tasks, adjusting vehicle capacities, and making minimal tweaks to accommodate the change. For example, if a dialysis patient isn’t ready for pickup at 2:00 p.m., the system can redirect the driver to handle a nearby urgent trip, ensuring efficiency before circling back once the patient is ready.
In emergencies like a vehicle breakdown, dispatchers can quickly identify available vehicles within a 3-mile radius. This allows them to assign the nearest driver to handle a critical pickup - such as a dialysis appointment - without causing delays for other passengers.
These systems also play a key role in managing unpredictable return trips, where discharge times can vary due to clinical workflows. Instead of having drivers wait around, the software combines rider status updates with driver availability through unified readiness signals. Once a patient is ready, the system dispatches the closest available vehicle, cutting down on wait times and improving overall efficiency.
Geofencing adds another layer of precision by creating virtual boundaries around facilities. When vehicles enter or exit these zones, the system logs the event and sends notifications to the appropriate parties. Dispatchers can even set up webhooks to get instant alerts when specific conditions are triggered.
Tracking metrics like Return-Trip On-Time Performance (OTP), Average Dwell Time, and Exception Resolution Time helps measure how effectively these adjustments are minimizing disruptions.
Organizing patients based on recurring trip patterns takes efficiency to the next level. By grouping individuals with similar schedules and destinations, you can make better use of vehicle capacity and cut down on empty miles. For example, clustering patients from the same dialysis center or nursing home reduces fuel costs and improves on-time performance. This approach complements optimizing NEMT routes and scheduling, ensuring every trip contributes to better fleet utilization.
The numbers back this up. AI-driven scheduling can slash manual planning time by around 40%. On top of that, intelligent dispatching systems can improve fleet efficiency by 20% to 30%, allowing providers to manage up to 34% more trips without needing extra staff or vehicles. Strategic patient grouping doesn’t just save time - it transforms how your operation grows.
Different patient groups have specific transportation needs that impact trip planning. Here’s a closer look at a few common categories:
Once you’ve grouped patients, it’s essential to customize services to meet their specific needs. For dialysis patients, confirm all details - addresses, mobility requirements, and appointment times - before setting up a standing order. This prevents service disruptions. Regularly review schedules since treatment plans or clinic hours can change, and plan ahead for holiday closures to avoid unnecessary trips that waste resources.
Keep an eye on no-show trends. If a patient repeatedly misses a scheduled trip, adjust their standing order to avoid wasting time and fuel. Sending SMS or phone reminders can also cut down on no-shows and improve driver efficiency. Additionally, when grouping patients by mobility type - whether ambulatory, wheelchair, or stretcher - make sure they are assigned to the right vehicle to prevent overbooking and maintain safety. These small but critical adjustments not only improve patient satisfaction but also streamline operations and maximize fleet performance.
A well-rounded approach to technology and communication is at the heart of effective recurring transportation management. By combining advanced AI tools, clear communication channels, and personalized services, organizations can create a system that not only reduces costs but also improves reliability and, most importantly, patient health outcomes. Providers can further optimize these outcomes by using a patient load analyzer to ensure capacity matches demand.
For example, real-time GPS tracking and automated SMS reminders have proven to cut patient wait times dramatically - from over 30 minutes to less than 10. These kinds of improvements are essential, especially for patients needing time-sensitive treatments like dialysis or chemotherapy.
"Reliable transportation is a lifeline for frequent riders. For dialysis patients, missing even one treatment can have immediate health impacts." - RoutingBox
Customizing transportation services to cater to different patient needs - whether it’s for recurring dialysis treatments or physical therapy sessions - ensures a dependable and patient-centered experience. Research also shows that dependable transportation can boost treatment adherence by up to 40% and lead to a noticeable drop in hospital readmissions.
To keep recurring trips organized and avoid duplicates, consider using scheduling tools that offer recurrence schedules or repeat options. These features let you specify repeat days, set end dates, and even exclude certain dates. Additionally, automation tools can streamline the process by managing recurring schedules efficiently. They ensure trips are only created when needed, while still allowing for adjustments or cancellations. This approach helps maintain accuracy and eliminates the risk of duplicate entries.
To manage clinic delays effectively, it's essential to incorporate flexibility into scheduling and utilize tools for real-time coordination. For example, adjustable time windows can help absorb delays without throwing the entire schedule off track. Additionally, real-time communication between drivers and riders ensures everyone stays informed, allowing for quick route adjustments when needed. These approaches not only help maintain reliability but also reduce missed appointments and ensure a consistent level of service, even when clinics experience unexpected delays.
To cut down on no-shows for standing orders, consider implementing automated scheduling and reminder systems. These tools can help manage recurring rides while sending timely SMS or email reminders to patients. Adding real-time GPS tracking and updates ensures patients stay informed about their ride status, reducing uncertainty. Establishing clear cancellation policies and offering incentives for consistent attendance can further encourage reliability. By blending smart technology with effective communication, you can significantly reduce missed pickups and improve overall efficiency.

Gosh, have you looked at the healthcare forest lately? It’s vast, beautiful, and—if we’re being honest—a little bit tangled! For a long time, the folks in the Non-Emergency Medical Transportation (NEMT) thicket thought that simply having "digital" tools was enough. They traded their paper maps for glowing screens and felt as fast as Thumper on a spring morning.
But according to a recent deep-dive from Healthcare IT Today, just being digital isn't the same as being truly connected. To keep the whole meadow healthy, we need something much more powerful: Interoperability.
It’s easy to get "twitterpated" by a new app or a sleek dashboard. Many NEMT providers have successfully moved away from manual scheduling, which is wonderful! However, if that digital data stays locked inside one system, it’s like a squirrel hiding nuts and then forgetting where they are.
The article points out a startling reality: while 96% of healthcare leaders feel ready to adopt digital solutions, over 90% admit that interoperability is still a major barrier. When systems don't talk to each other, the "Great Prince" (that’s the patient!) ends up waiting in the cold.
In the old days, a transport provider might not know a patient’s specific needs until they arrived at the burrow. With true interoperability, information flows seamlessly between:
To make this happen, everyone in the forest needs to speak the same language. We aren't just talking about chirps and whistles; we’re talking about FHIR (Fast Healthcare Interoperability Resources) and standardized APIs. These tools allow different systems to "shake paws" and share data without any "stags" getting in the way of progress.
The healthcare forest is changing, and we can’t just stand still like a deer in headlights! Moving beyond "digital" and toward a fully interoperable standard is the only way to ensure every patient reaches the meadow safely and on time.
It’s time to stop building fences around our data and start growing a connected ecosystem where information—and patients—can move freely.

The Transportation Alliance Foundation just dropped a landmark study on how outdated regulations are hurting for-hire transportation providers — and NEMT operators should be paying close attention.
Published: February 2026 | Category: Industry News & Regulation | Read time: ~8 min
If you run a non-emergency medical transportation company, you already know the regulatory landscape feels like it was designed for a different era. You’re juggling Medicaid contracts, commercial insurance mandates, vehicle inspections, and licensing requirements that seem to multiply every time you cross a county line.
Now there’s a major new report that puts hard data and real-world case studies behind what many of you have been saying for years: the rules aren’t fair, and they’re holding the industry back.
In January 2026, The Transportation Alliance Foundation (TTAF) and the University Transportation Research Center (UTRC) at the City College of New York published “Mobilizing for Fair Regulation & Competition with Transportation Network Companies (TNCs)” — a comprehensive study examining how outdated regulations create an uneven playing field between traditional for-hire vehicle operators (taxis, limousines, and yes, NEMT providers) and app-based platforms like Uber and Lyft.
The report was authored by Matthew W. Daus, Esq., a nationally recognized transportation law expert and former NYC Taxi & Limousine Commissioner. While the study primarily targets taxi and limousine policy, the implications for NEMT operators are significant. Let’s break down what it means for your business.
The report’s central finding is straightforward: traditional transportation providers — taxis, limousines, and the fleets that many NEMT companies operate — are regulated under a patchwork of strict local rules, while TNCs like Uber and Lyft operate under lighter, statewide frameworks. According to the study’s industry surveys, over 73% of taxi respondents said TNCs are either more popular than or directly competing with their services, and nearly 58% of limousine operators agreed.
For NEMT providers, this regulatory imbalance might feel familiar. You’re required to maintain commercial vehicle registrations, carry full-time commercial insurance (often 24/7, regardless of whether you’re on a trip), pass rigorous vehicle inspections, and comply with strict driver background check requirements. Meanwhile, TNC drivers can sign up through an app and hit the road with far fewer hurdles.
The report specifically acknowledges that NEMT companies were invited to participate in the research, noting that their operational context “differs substantially” from traditional for-hire sectors because NEMT concerns are predominantly contract-driven. The study recommends future research to examine NEMT-specific contractual, reimbursement, and procurement dynamics — a recognition that our sector needs and deserves its own focused analysis.
If insurance premiums keep you up at night, you’re not alone. The report identifies insurance as one of the single largest cost burdens facing for-hire transportation operators. Among limousine companies surveyed, 57% rated insurance as a high-impact burden. One fleet operator described their premiums as “absolutely ridiculous — over $300K per year for 11 vans.”
Here’s the kicker: while you’re paying for 24/7 commercial coverage whether your vehicles are running trips or sitting in a lot, TNCs use a tiered, period-based insurance system. When a TNC driver’s app is off, their personal auto policy applies. When they’re waiting for a ride, limited coverage kicks in. Full commercial coverage only applies once a passenger is in the vehicle.
The report highlights Arizona as a model worth studying. Under Arizona’s framework (Ariz. Rev. Stat. § 28-4039), taxis, limousines, and TNCs all operate under period-based insurance. When a driver is simply available but not on a trip, lower coverage limits apply. Higher limits kick in only when a ride is accepted and in progress. This approach was adopted in 2015 and has been widely praised for reducing costs while maintaining safety.
What this means for NEMT: If your state adopted a similar model, you could potentially see significant savings on premiums during downtime between Medicaid trips. The report found that 60% of taxi respondents and 58% of limousine respondents support insurance requirements that vary based on driver status. This is a policy shift worth advocating for.
Many NEMT providers operate wheelchair-accessible vehicles (WAVs) that represent a serious capital investment. The report argues that rigid vehicle age caps — common in taxi and limo regulations — are outdated and actively harmful. These rules force operators to retire vehicles based on age rather than condition, driving up fleet turnover costs and discouraging investment in expensive WAVs, electric vehicles, and hybrids.
Washington, D.C. provides a promising case study. The D.C. Department of For-Hire Vehicles (DFHV) has progressively extended vehicle retirement ages: from 8 years to 10 (in 2020), then to 15 years for internal combustion vehicles and a full 20 years for EVs, hybrids, and WAVs (in 2024). They also eliminated a 300,000-mile cap and replaced the old waiver-request system with a predictable annual suitability review.
What this means for NEMT: If your jurisdiction has strict vehicle age limits, the report’s recommendations could support your advocacy for condition-based inspections instead. A well-maintained WAV at 12 years old is far more valuable to the community than forcing an operator to replace it at 8 years — especially when a new WAV can cost $50,000 to $80,000 or more.
NEMT providers often transport patients across city and county lines — to specialist appointments, dialysis centers, or hospitals in neighboring jurisdictions. But while an Uber driver can seamlessly pick up passengers anywhere in the state, many for-hire vehicle operators need separate licenses for each jurisdiction.
The report makes a strong case for permit reciprocity. Over 54% of taxi survey respondents strongly support regional reciprocity, and the study highlights several real-world success stories. Florida’s Statute § 320.0603 (effective July 2024) now allows limousine businesses to operate anywhere in the state with a single home-jurisdiction permit. California’s Government Code § 53075.51(d) requires cities within the same county to recognize each other’s taxi permits.
What this means for NEMT: If you serve a metro area that spans multiple cities or counties, reciprocity legislation could eliminate duplicative licensing fees, reduce administrative burden, and allow you to serve more patients more efficiently. The report provides ready-made policy language and case studies you can share with your local representatives.
One of the report’s more encouraging findings is about technology adoption. The study notes that many traditional taxi operators are still relying on phone dispatch and cash payments — over 50% of taxi business still comes from call-ins or street hails. The report recommends that regulators allow “soft meters” (GPS-based fare calculation on tablets or phones), upfront pricing, and e-hail apps.
The good news for NEMT providers? If you’re already using modern dispatch and scheduling software like Bambi, you’re ahead of the curve. Automated scheduling, AI-optimized routing, real-time GPS tracking, and digital trip management aren’t just nice-to-have features — they’re exactly the kind of technology this report says the entire for-hire industry needs to adopt to stay competitive. San Francisco’s Taxi Upfront Fare Program saw a 25% increase in average driver earnings after modernizing, and driver applications surged fivefold.
What this means for NEMT: The regulatory winds are shifting toward technology-enabled transportation. Providers who have already invested in modern platforms are well-positioned to demonstrate compliance, efficiency, and accountability to Medicaid brokers and regulators alike.
The report digs deep into the disparity in wheelchair-accessible vehicle (WAV) obligations. Under the ADA, taxis are required to acquire accessible vehicles if they buy new vans, and many cities impose additional WAV fleet mandates. TNCs, by contrast, don’t own vehicles — so WAV acquisition rules simply don’t apply to them. The report recommends standardizing accessibility requirements across all provider types.
What this means for NEMT: NEMT providers who maintain WAV fleets carry a significant cost burden that TNCs don’t share. The report’s push for equalized accessibility expectations could eventually create a more level competitive environment. If you operate WAVs, this is powerful ammunition for conversations with state legislators about the costs of providing these essential services.
Over 50% of limousine respondents and 37% of taxi respondents identified illegal and unlicensed operators as a major challenge. The report describes a troubling ecosystem: unlicensed drivers avoiding insurance, background checks, and inspections while undercutting compliant businesses on price.
What this means for NEMT: In the NEMT space, this translates to providers who may cut corners on driver qualifications, vehicle maintenance, or insurance — putting vulnerable patients at risk while underbidding compliant operators on Medicaid contracts. The report’s recommendation for stronger enforcement tools (centralized licensing databases, GPS verification, automated insurance validation) would benefit every NEMT provider who plays by the rules.
This report gives you a concrete toolkit for advocacy. Here are the key steps:
This TTAF/UTRC report is a wake-up call for the entire for-hire transportation industry, and NEMT providers have a unique stake in its recommendations. The regulatory imbalances it identifies — in insurance, licensing, vehicle standards, technology access, and accessibility requirements — all directly impact NEMT operations and profitability.
The good news? The report doesn’t just diagnose problems. It provides actionable policy recommendations, real-world case studies, and survey data you can use to advocate for change. And the report itself acknowledges that NEMT deserves dedicated research — a signal that the industry’s unique challenges are finally being recognized at the national policy level.
Fairer regulations, smarter insurance models, and technology-forward policies aren’t just good for the industry — they’re good for the patients and communities NEMT providers serve every day.
Original Report: “Mobilizing for Fair Regulation & Competition with TNCs” — The Transportation Alliance Foundation & University Transportation Research Center (January 2026)
Organizations & Institutions:
Regulatory Case Studies Referenced:
NEMT Industry Resources:
— — —
Ready to modernize your NEMT operations?
See how Bambi’s AI-powered dispatch and scheduling platform can help you run more trips, cut costs, and stay ahead of regulatory changes. Get started at hibambi.com
.png)
See the full interview on YouTube
Please don't forget to subscribe and like NEMT Experts Podcast on YouTube.
Also, available to watch on Spotify
And listen (audio only) on your other favorite podcast platforms Apple and Pandora.
In this Episode 104 of the NEMT Experts Podcast, we talk with Thomas Clancy, VP at Research Underwriters, a longstanding insurance broker in the transportation industry, on what NEMT business owners need to know in 2026 about getting the insurance they need in order to operate.Top 3 quotes
1. Work with an NEMT-specialist broker
Tom’s point: insurance is too niche to “wing it” with someone who doesn’t live in transportation. The right broker helps you get correct coverages, meet contract requirements, and acts like an advisor as you grow.
2. The “must-have” coverage stack in 2026
He calls out Auto Liability + General Liability + Molestation as the core trio. The big idea: each covers different risk, and gaps are where lawsuits love to move in rent-free.
3. Safety tech + driver training can meaningfully impact underwriting.
Cameras (forward + rear facing), telematics, routing software, and documented driver training help reduce claims and help a broker present you as a “good risk.” He also stresses: don’t just “install cameras to check a box”… actually use the data for coaching.