Starting a business in the healthcare transportation sector can feel overwhelming, especially when you’re figuring out how to structure your ideas. That’s where a tool like our NEMT Business Plan Generator comes in handy. It’s designed to help aspiring entrepreneurs map out their vision for providing essential transport services to those who need it most, whether it’s elderly individuals or folks in underserved areas.
A well-thought-out plan is your first step toward turning a compassionate idea into a sustainable operation. By focusing on key elements like your target audience and operational needs, you can identify potential challenges early—like securing vehicles or navigating regulations. Our free resource simplifies this by creating a custom outline that reflects your specific goals and service region, saving you hours of research.
Beyond just generating a document, this tool empowers you to think critically about your startup’s future. Pair it with local market research and expert advice, and you’ll be well on your way to making a real difference in your community through accessible transportation solutions.
This tool is designed for entrepreneurs and small business owners who want to start a non-emergency medical transportation company. Whether you’re targeting elderly clients, people with disabilities, or rural communities, it helps you create a basic plan to organize your thoughts and present to potential investors or partners. It’s perfect for those just starting out who might not have the budget for a professional consultant yet.
The plan you get is a solid starting point, customized to the details you provide, like your service area and target market. It includes key sections such as an Executive Summary and Operational Plan with templated content to guide you. That said, it’s not a substitute for professional advice—think of it as a framework you can build on with input from financial or legal experts.
Absolutely! The output is fully editable, so you can tweak any section to better fit your vision or add more specific details. We even include placeholders in the text to suggest where you might want to dive deeper. Once generated, copy it into your favorite word processor or keep refining it as your business idea evolves.

Publish Date: November 5, 2025.
Strategic partnership combines innovative fleet technology with transportation benefit management expertise to improve medical transportation coordination
Non-emergency medical transportation (NEMT) just got smarter and simpler. Bambi, a leading NEMT software platform, has integrated with Provide A Ride, a prominent NEMT transportation benefit manager serving managed care organizations and state Medicaid agencies.
The integration connects Bambi's dispatch, routing and fleet management technology directly with Provide A Ride's operations, creating a seamless flow of information between transportation providers and the benefit manager. This means faster trip assignments, real-time visibility into vehicle locations, and better coordination for the Medicaid members who depend on these rides to reach critical medical appointments.
NEMT serves a vital role in healthcare access. Millions of Medicaid beneficiaries rely on these rides to get to dialysis appointments, chemotherapy treatments, primary care visits, and other essential medical services. When transportation breaks down, so does the care continuum.
The challenge? Coordination. Traditional NEMT systems often involve phone calls, faxes, and manual data entry between brokers and transportation providers. This creates delays, miscommunication, and gaps in service.
The Bambi and Provide A Ride API integration eliminates these friction points. Transportation providers using Bambi can now receive trip assignments from Provide A Ride directly through their software, and share live updates on trip status without picking up a phone or sending an email.
Transportation providers who use Bambi's dispatch software can connect their system to Provide A Ride's network through a secure API integration. Once connected:
The result is a streamlined workflow that reduces response times, improves service reliability, and frees staff to focus on member care rather than paperwork.
Alan Groedel, President of Provide A Ride, sees the partnership as a strategic move to strengthen every part of the transportation ecosystem.
"At its core, NEMT is about closing gaps—gaps in access, experience, and insight," Groedel said. "Our partnership with Bambi helps close those gaps in real time, pairing best-in-class technology with the hands-on expertise that defines Provide A Ride. This collaboration strengthens every link in the chain, from our clients to our transportation partners to the members we serve, delivering smarter coordination, faster response, and a more human experience."
Nirav Chheda, CEO of Bambi, emphasized the importance of creating technology that works for the people on the ground.
"Transportation providers shouldn't have to choose between great service and efficient operations," Chheda said. "Our integration with Provide A Ride proves that technology can support both. By connecting our platform directly with one of the most respected brokers in the industry, we're helping providers spend less time on administrative tasks and more time getting members to their appointments safely and on time."
For the small and mid-sized transportation companies that form the backbone of NEMT service delivery, this integration offers tangible benefits:
Reduced administrative overhead. No more manually entering trip details from emails or phone calls. Assignments arrive in the system ready to dispatch.
Faster trip acceptance. Providers can evaluate and accept trips in seconds, improving their competitiveness and fill rates.
Better utilization. Real-time visibility into trip availability allows providers to optimize routes and maximize vehicle use.
Simplified compliance. Automated trip documentation and reporting help providers meet contract requirements without additional data entry.
Managed care organizations and state Medicaid agencies benefit from improved network performance. The integration provides health plans with better visibility into their transportation network, more accurate trip tracking, and data-driven insights into service quality.
For the members who rely on these rides, the benefits are direct: shorter wait times, more reliable pickups, and a better overall experience. When technology reduces friction in the system, the people at the end of that system get better service.
The integration is live and available to transportation providers in Provide A Ride's network. Providers interested in connecting their Bambi software to Provide A Ride's system can contact Bambi for technical onboarding support.
As NEMT continues to evolve with technology, partnerships like this one set a new standard for how transportation brokers and providers can work together with the help of leading NEMT technology like Bambi. The focus remains clear: use technology to remove barriers, not create them, so that every member gets the ride they need when they need it.

Bambi provides dispatch and fleet management software designed specifically for NEMT providers. The platform helps transportation companies manage scheduling, routing, driver communication, billing, and compliance from a single system. Bambi serves providers ranging from small owner-operators to regional fleets across the United States.
Learn more at: https://www.bambinemt.com/

Provide A Ride is a trusted partner in non-emergency medical transportation, serving managed care organizations and state Medicaid agencies with a hybrid model that integrates transportation benefit management services and direct fleet operations. With a focus on transparency, retention, and service excellence, Provide A Ride helps health plans meet their members where they are and get them where they need to go.
Learn more at: https://providearide.com/
Media Contact:
For more information about this partnership, contact Bambi at info@bambinemt.com or Provide A Ride through their website at provideride.com.
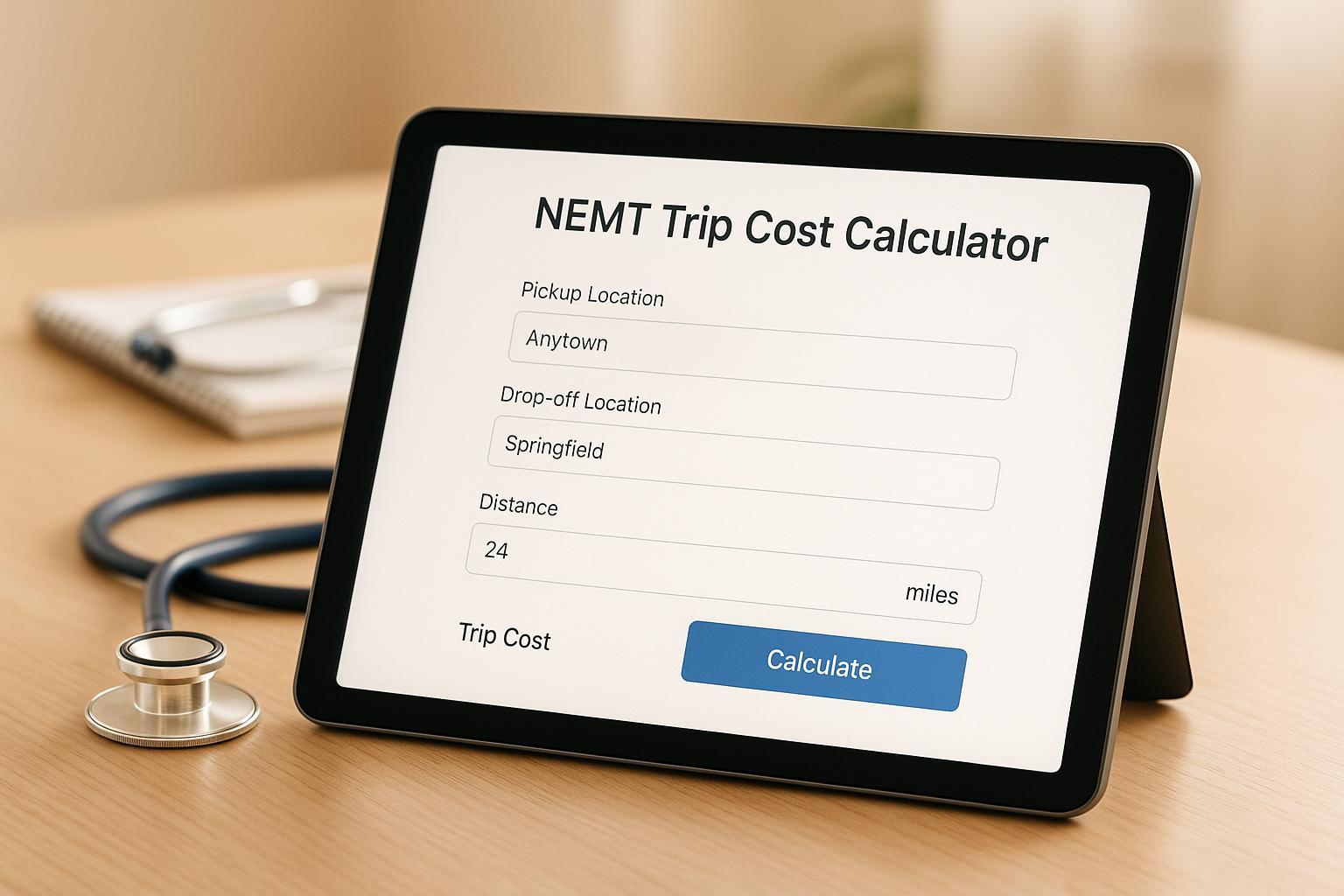
Navigating the world of non-emergency medical transportation (NEMT) can feel overwhelming, especially when it comes to budgeting for trips to doctor’s appointments, therapy sessions, or other healthcare needs. That’s where a reliable NEMT trip cost estimator comes in handy. This tool simplifies the process by letting providers and clients calculate expenses based on distance, rates, and additional services, ensuring transparency every step of the way.
For many, planning a ride for medical purposes isn’t just about logistics—it’s about peace of mind. Knowing the potential expenses upfront helps families and caregivers make informed decisions without last-minute surprises. Whether it’s factoring in mileage rates or accounting for special assistance fees, having a clear picture of healthcare transport pricing can ease the burden. Plus, with features like discounts for multiple passengers, tools like these cater to real-world scenarios, making them invaluable for both individuals and businesses in the NEMT space. So next time you’re scheduling a ride, take a moment to crunch the numbers—it’s a small step that can save time and stress.
It’s pretty straightforward! The tool multiplies the trip distance by the cost per mile—defaulting to $2.50 if you don’t specify a rate. Then it adds any extra fees for things like waiting time or special assistance. If you’ve got two or more passengers, it applies a 10% discount to the total. You’ll see every part of the calculation broken down clearly, so there’s no mystery.
Absolutely, and it’s even better with more people! Just enter the number of passengers, and if it’s two or more, the tool automatically applies a 10% discount to your total cost. It’s a nice little perk for group trips, and the final breakdown will show exactly how much you’re saving.
No worries—we’ve got you covered. If you accidentally input something like a negative number or non-numeric value for distance, cost, or fees, the tool will display a friendly message saying, 'Please enter valid numbers.' Just double-check your entries, and you’ll be good to go in no time.
.png)
See the full interview on YouTube
Please don't forget to subscribe and like NEMT Experts Podcast on YouTube.
Also, available to watch on Spotify
And listen (audio only) on your other favorite podcast platforms Apple and Pandora.
In this Episode 93 of the NEMT Experts Podcast, we talk with Derrick Kirunda, the owner of Care Route Medical Transportation, a fast-growing NEMT business in Seattle, WA, on how he's been able to win facility contracts so quickly.
Be ready and you win the moment. A competitor was exposed for no insurance and the hospital moved all rides to Care Route overnight. Because licenses, insurance, and vehicles were ready, Derek captured the work and doubled the fleet fast by renting short term, then financing more vans.
Make it easy for facilities. Most partners don’t even use a formal contract. They book through Bambi’s portal, get confirmations, and Care Route accepts ~90% of requests. Reliability, branded vehicles, and Google reviews feed steady private and facility demand.
Grow where others hesitate. Non-emergency discharges via Broda chairs and stretcher work are profitable and practical. Care Route trained and certified for stretchers, priced Broda correctly, and aims to be the Seattle region’s go-to for hospital discharges.
“They terminated the contract and the next company they called was Care Route. We were ready.”
“Most facilities don’t need a formal contract. They book in Bambi and 90% of the time we take it.”
“If a patient is discharging, they don’t need an ambulance.”
.png)
See the full interview on YouTube
Please don't forget to subscribe and like NEMT Experts Podcast on YouTube.
Also, available to watch on Spotify
And listen (audio only) on your other favorite podcast platforms Apple and Pandora.
In this Episode 92 of the NEMT Experts Podcast, we talk with Tony Aycock, Senior Manager of Transportation at Call The Car, a large broker and transportation provider in California, on how they complete nearly one million NEMT rides every month.
1. Technology is the engine of scale.
Call the Car handles nearly one million rides per month by fully embracing technology — from real-time APIs to AI-powered dispatching. Transitioning to Bambi’s system drastically improved on-time performance, reduced workload, and enabled smarter, data-driven routing.
2. Automation multiplies efficiency — if you trust it.
Before switching to AI-based optimization, Call the Car used up to eight dispatchers daily just to manage routing. Now, only two handle the entire fleet, while others focus on subcontractor coordination. The hardest part wasn’t the tech — it was letting go of manual control and trusting automation.
3. Growth comes from doing what others avoid.
Tony’s biggest advice to providers: take the trips no one else wants. Focus on underserved categories (like wheelchair or lower-level ambulatory rides), do them exceptionally well, and use tech to stay profitable. That’s how you build credibility and long-term contracts with brokers.
“Anyone who’s willing to embrace technology are the companies that are going to springboard into the future.”
“We went from seven or eight dispatchers down to two — and every time we trust the AI to handle it, it works out really well.”
“Do the things nobody else wants to do, and do them really well. That’s how you become the go-to provider for brokers.”
.png)
Uber vs NEMT vs Ambulance — what's the future for NEMT?! | NEMT Experts Podcast Episode 91
See the full interview on YouTube
Please don't forget to subscribe and like NEMT Experts Podcast on YouTube.
Also, available to watch on Spotify
And listen (audio only) on your other favorite podcast platforms Apple and Pandora.
In this episode of the NEMT Experts Podcast, Nirav sits down with Dominic Buono, the Director of Business Development at Onward, who lays out the emerging trends of how NEMT is stacking up to TNCs like Uber and Lyft and to ambulance companies.

NEMT software is critical for managing patient transportation but often falls short due to outdated systems, compliance risks, and integration issues. Providers face challenges like scheduling errors, data security concerns, and user resistance, which lead to inefficiencies and poor patient care.
Modern NEMT tools, like automated scheduling and self-service portals, can reduce no-show rates by up to 40% and improve efficiency. Investing in secure, easy-to-use software ensures better service and long-term growth.
NEMT providers often face recurring software challenges that disrupt operations and impact patient care. Let’s explore the key issues and how to address them effectively.
Many NEMT providers still rely on manual scheduling methods, such as pen-and-paper logs or basic spreadsheets. These older systems lead to inefficiencies, errors, and delays that can ripple through the entire operation.
Manual data entry is prone to mistakes like double-bookings, missed appointments, and poorly planned routes. Without real-time updates, dispatchers struggle to respond to delays or cancellations, leaving staff bogged down in administrative tasks instead of focusing on patient needs.
The solution? Transition to cloud-based platforms with integrated scheduling and dispatch features. Modern NEMT software prevents overbooking, provides real-time updates across devices, and includes GPS tracking for optimized route planning. Look for systems with automated fleet management, self-service booking portals, and direct communication tools for drivers and passengers. These features streamline operations and improve the overall experience for both staff and patients.
NEMT software deals with sensitive patient data, making data security and HIPAA compliance a top priority. Unfortunately, many providers struggle with weak encryption, inadequate access controls, and systems that fail to meet federal privacy standards. Data breaches in healthcare can result in hefty fines and long-term damage to a provider's reputation.
Common vulnerabilities include unencrypted data transmission, lack of multi-factor authentication, and insufficient access monitoring.
To address these issues, adopt platforms with strong encryption for data storage and transmission. Key features should include multi-factor authentication, role-based access controls to limit staff access, and audit trails to monitor system activity. Work with vendors that have proven expertise in healthcare data security and can provide compliance certifications. Regular third-party security audits, along with staff training on HIPAA requirements, are also crucial for maintaining a secure system.
While upgrading scheduling systems improves efficiency, integration issues can create new problems. Many NEMT providers face difficulties connecting their legacy systems - like billing tools, fleet management software, and HR platforms - with modern NEMT solutions. These compatibility issues often lead to data silos and workflow disruptions.
When systems don’t communicate effectively, staff may need to manually transfer data, increasing the risk of errors and doubling their workload.
To avoid these headaches, choose software with open APIs and flexible integration options. Prioritize solutions that enable seamless data sharing with your existing systems. Collaborate closely with your IT team and the software vendor to plan a phased integration. Start with non-critical systems to identify potential issues before rolling out full implementation. For example, Bambi actively works to integrate with major ride brokers and customizes connections based on provider needs.
Even the most advanced software can fail if it’s difficult to use. Complex interfaces and poorly designed systems often lead to staff frustration, resistance, and low adoption rates. Employees accustomed to manual processes may hesitate to switch, especially if the new system feels overwhelming or doesn’t clearly improve their workflow.
Resistance tends to stem from fear of change, inadequate training, or software that complicates rather than simplifies tasks. When employees don’t see the benefits or feel unsupported, they may revert to old methods, undermining the upgrade.
To overcome this, invest in user-friendly software with intuitive navigation and customizable dashboards that align with your team’s needs. Involve staff in the selection process so they can test options and provide feedback. Offer comprehensive training that highlights how the system will make their daily tasks easier, not just how it works. Provide ongoing support and designate internal champions who can assist colleagues during the transition. Sharing success stories and demonstrating efficiency gains can help maintain enthusiasm.
For many NEMT providers, high upfront costs and ongoing subscription fees are major hurdles. Smaller operations, in particular, may struggle to justify the expense, especially if the return on investment (ROI) isn’t immediately clear.
Some providers focus only on the initial price tag, overlooking the total cost of ownership, which includes training, integration, and long-term support. Others opt for cheaper solutions that lack critical features, leading to additional expenses later.
To make smarter financial decisions, consider the full picture. Calculate how much manual processes currently cost in terms of staff time, errors, and missed opportunities. Factor in potential savings from reduced no-shows, better route efficiency, and lower administrative overhead. Look for vendors offering scalable pricing models that grow with your business. Some providers offer tiered plans, allowing you to start with basic features and expand as needed. Request detailed ROI projections and references from providers of similar size to understand their real-world results.
Skipping upgrades can lead to hidden costs, including compliance risks, operational inefficiencies, and higher staff turnover. Addressing these challenges head-on ensures smoother operations and better patient care.
NEMT providers often face daily operational challenges that hinder staff productivity and patient satisfaction. Issues like manual data entry and outdated communication methods contribute to scheduling errors and billing mistakes, creating inefficiencies that ripple through the entire service process.
Take manual data entry, for instance. Dispatchers often spend hours inputting trip details, client information, and billing data into spreadsheets or paper-based systems. This approach not only eats up valuable time but also increases the likelihood of errors. Mistakes in scheduling or billing can lead to denied insurance claims, lost revenue, and compliance risks. On top of that, the labor costs associated with these manual processes cut into profit margins, diverting resources from more critical tasks.
Communication gaps make things even worse. Relying on phone calls or text messages for updates between dispatchers, drivers, and patients often results in delayed responses and missed information. Patients are left uninformed about trip statuses, and when drivers can’t quickly communicate delays or cancellations, the result is frustration and strained relationships.
The absence of real-time tracking compounds these problems. Without GPS tracking and automated updates, dispatchers are often in the dark about vehicle locations or trip progress until it’s too late to address an issue. This lack of visibility undermines service quality and leads to preventable disruptions.
Modern software solutions are changing the game by automating processes and improving communication. For example, automated SMS and app alerts keep patients informed about pickup times and schedule changes, which significantly reduces no-show rates. Real-time GPS tracking provides immediate updates on vehicle locations, traffic conditions, and estimated arrival times, helping dispatchers and drivers stay aligned.
AI-powered dynamic scheduling takes things a step further by analyzing trips and recommending optimal assignments. This minimizes the need for manual trip allocation, saving time and reducing errors. As one user, Julian from Bellshan Homecare, shared:
"How much time it saves me? It's like a day's worth of time. And sometimes once I make the dispatch the system just does the work, so I don't have to sit on the computer all day trying to see where the driver is."
– Julian, Bellshan Homecare
Self-service booking portals also play a big role in improving efficiency. These portals allow customers to schedule, track, and manage their rides on their own, reducing the administrative workload for dispatchers while giving patients greater control and visibility over their trips.
Integrating with NEMT brokers is another key improvement. By enabling direct data exchange with major ride brokers, providers can automate the import of trip requests, cutting down on manual data entry and speeding up the scheduling process. This reduces errors and allows dispatchers to focus on higher-value tasks.
Alex Stoia from Corazon Concierge highlighted the transformative impact of advanced scheduling and tracking systems:
"Integrating advanced scheduling software and real-time tracking systems has revolutionized how we operate. Our efficiency has improved dramatically, leading to better service for our clients."
– Alex Stoia, Corazon Concierge
To make the most of these tools, it’s essential to track performance metrics like on-time rates, no-show and cancellation rates, average response times, and data entry error frequency. Monitoring these metrics helps providers pinpoint bottlenecks and measure the effectiveness of operational changes.
Finally, successful implementation requires careful planning. Providers should select platforms that not only offer comprehensive automation features but also ensure HIPAA compliance with robust encryption and secure access controls. For more practical tips on integrating these systems, check out the Bambi NEMT blog (https://hibambi.com).
Here’s a breakdown of some common challenges in NEMT software, their impacts, and how modern solutions tackle these issues:
| Problem | Operational Impact | Solution | Expected Results |
|---|---|---|---|
| Outdated Scheduling & Dispatch Systems | Issues like double-booking, late pickups, inefficient routing, and wasted staff hours | Cloud-based platforms with AI-driven scheduling, automated notifications, and real-time GPS tracking | Fewer scheduling errors, better route efficiency, and significant time savings (up to a full day per dispatcher) |
| Data Security & HIPAA Compliance Issues | Risks of legal penalties, data breaches, and loss of patient trust | Secure encryption, access controls, regular audits, and HIPAA-compliant platforms | Stronger data security and reduced compliance risks |
| Integration & Compatibility Problems | Data silos, workflow disruptions, manual data re-entry, and billing delays | Open API software with broker integrations and strong customer support | Smoother data flow, automated trip processing, and lower administrative burden |
| Poor User Experience & Staff Resistance | Low adoption rates and higher training costs slowing digital adoption | Easy-to-use interfaces, thorough staff training, and involving users in software selection | Improved adoption rates, higher productivity, and shorter training periods |
| Cost & Budget Barriers | Limited adoption of technology, reliance on manual systems, and higher operational expenses | Scalable pricing options (e.g., $69/month/vehicle) and clear ROI analysis | Predictable costs with measurable efficiency improvements |
| Lack of Operational Visibility | Weak fleet management, billing errors, and difficulty tracking driver locations or trip progress | Real-time GPS tracking, centralized dashboards, and automated updates | Better fleet oversight, fewer billing disputes, and improved communication with customers |
| Fraud & Abuse Risks | Financial losses due to false claims, compliance violations, and reputation damage | GPS-verified trip records, fraud monitoring tools, and detailed audit trails | Reduced fraud, increased accountability, and stronger compliance documentation |
This table highlights the core issues and how modern solutions can address them effectively. These challenges not only disrupt daily operations but also hit revenue and service quality hard. For instance, late arrivals and no-shows are among the most frequent complaints from NEMT users, directly affecting both patient satisfaction and revenue streams. Manual scheduling systems often lead to drivers showing up at the wrong time - or not at all - which can compromise patient care.
The solutions outlined above, like real-time scheduling and GPS tracking, have been shown to significantly cut down on late arrivals and improve route efficiency. Providers who have adopted these advanced systems report noticeable improvements in operational efficiency and overall service quality.
A major takeaway here is the importance of choosing platforms that address multiple challenges at once. As highlighted by industry experts, including insights from the Bambi NEMT blog (https://hibambi.com), comprehensive platforms powered by AI can optimize dispatching, scheduling, compliance, and communication while improving efficiency and patient care.
When considering solutions, it’s smart to look beyond upfront costs. Platforms with transparent pricing structures and features like broker integrations and automated scheduling often deliver measurable time and cost savings, making the investment worthwhile.
Tapping into expert resources can turn operational hurdles into streamlined solutions. One great example is the Bambi NEMT blog (https://hibambi.com), a dedicated platform created to support NEMT providers. This blog doesn’t just identify common challenges - it offers actionable solutions tailored to the industry.
The blog dives into key areas like funding strategies, fleet management, driver training, and how technology can tackle persistent issues like routing inefficiencies and no-shows. By addressing these real-world problems, it connects directly to the operational challenges NEMT providers often face, offering practical advice that makes a tangible difference.
For those transitioning from manual processes to automated platforms, the blog provides step-by-step guidance. Topics like advanced integration testing and post-implementation monitoring are covered in detail, ensuring system stability after upgrades.
Managing change is another focus area, with strategies to help providers overcome staff resistance. Suggestions like involving team members in system selection and rolling out changes in phases can make the adoption process smoother.
Real-world success stories further illustrate the benefits of adopting modern technology. For example, providers who upgraded their systems reported fewer missed rides, quicker billing cycles, and happier drivers. One former NEMT driver shared their experience with the Bambi Driver App, noting how its user-friendly design reduced errors and boosted overall efficiency.
The emphasis on user-friendly technology is a recurring theme. Drivers frequently highlight how intuitive tools like the Bambi Driver App simplify their work compared to older, more cumbersome software. This shows how the right technology can actually reduce complexity instead of adding to it.
Beyond software, these resources keep providers informed about regulatory updates and best practices. Staying up-to-date on HIPAA compliance and other evolving standards is critical to avoiding penalties and maintaining smooth operations.
For those navigating the crowded landscape of technology options, expert guidance helps cut through marketing noise. The focus on AI-driven automation and scalable cloud-based platforms reflects the industry’s shift toward smarter, more adaptable solutions that grow alongside businesses.
The true value of these resources lies in their industry-specific expertise. Unlike generic business advice, they address the unique needs of NEMT operations, from broker integrations to GPS-verified trip records. This depth of knowledge is essential for providers looking to optimize their services.
Addressing common challenges in NEMT software can completely change how your operation runs. Moving from outdated, manual systems to automated, cloud-based platforms can cut no-show rates by up to 40% and reduce late pickups by 30%.
Failing to tackle these issues often leads to hidden labor costs, more frequent errors, and risks of noncompliance that can result in hefty fines and strained relationships with healthcare partners. On the other hand, investing in modern NEMT software usually pays off by lowering operational costs, minimizing missed appointments, and boosting overall efficiency.
Concerns from staff, such as resistance to new technology, tend to fade when providers choose user-friendly platforms and involve their teams early in the decision-making process. Many drivers who were initially hesitant about adopting new systems have found that intuitive technology actually makes their jobs easier, reducing both frustration and mistakes. This proves that the right tools simplify workflows instead of complicating them.
By upgrading to cloud-based, automated platforms, providers not only streamline their current operations but also set themselves up for long-term growth. Sticking with outdated systems, however, can hold back progress.
For expert advice and actionable insights, turn to resources like the Bambi NEMT blog. It’s packed with practical solutions, regulatory updates, and success stories tailored specifically to the NEMT industry - offering guidance that generic business advice simply can’t provide.
To meet HIPAA requirements and keep sensitive data secure, NEMT providers should rely on software equipped with strong security measures like encrypted communication, secure data storage, and role-based access controls. These tools are essential for protecting patient information and staying within regulatory guidelines.
Beyond choosing the right software, it's equally important to keep it updated, provide staff with training on data privacy best practices, and perform routine audits to spot and fix any weaknesses. Incorporating modern AI-driven tools can also streamline operations while ensuring compliance with HIPAA standards.
Switching from manual scheduling to cloud-based software in NEMT operations brings a range of benefits that can transform how businesses manage their daily tasks. These platforms streamline trip scheduling and fleet management by automating processes with advanced tools like AI, cutting down on human errors and saving valuable time.
This shift can boost efficiency, enabling businesses to manage more trips while using fewer resources. On top of that, many users find these platforms easy to navigate and appreciate the responsive customer support teams that help ensure a seamless transition. By adopting cloud-based systems, NEMT services can improve both operational workflows and the overall experience for their customers.
Implementing new software often comes with its share of challenges, especially when staff members resist the change. This hesitation usually stems from concerns about added workload or simply feeling unsure about how to use the new system. The key to overcoming this is clear and open communication. Highlight the benefits - like increased efficiency, streamlined scheduling, and fewer manual tasks - to help your team see the value it brings to their daily work.
Hands-on training and ongoing support play a crucial role in easing the transition. When employees feel equipped and supported, they're more likely to embrace the new tools. For instance, user-friendly platforms such as Bambi are built to simplify operations. With features like automated trip assignments and an intuitive interface, software like this can not only make adoption easier but also enhance the overall efficiency of your team's workflows.

Auditors evaluating Non-Emergency Medical Transportation (NEMT) providers focus heavily on documentation to ensure compliance with Medicaid and state regulations. Missing or incomplete records can lead to penalties, denied claims, or even exclusion from Medicaid programs. Here are the 5 key documents auditors typically request:
Key Takeaway: Accurate, organized, and up-to-date documentation is critical for passing audits. Digital tools can simplify compliance management, reduce errors, and ensure records are easily retrievable during audits. Missing any of these documents can result in fines, claim denials, or operational disruptions.
PCS forms play a key role in confirming the medical need for each Non-Emergency Medical Transportation (NEMT) trip. These forms document a licensed provider's assessment, ensuring that the service is medically justified. Without them, auditors may struggle to verify the legitimacy of claims, making PCS forms a critical piece of compliance.
Auditors often compare PCS forms with trip logs and billing records to uncover potential fraud or billing errors. These forms provide the medical justification required for Medicaid and Medicare reimbursements. Accuracy and completeness are non-negotiable when it comes to meeting compliance standards.
For a PCS form to meet compliance standards, it must include key details like the patient’s full name, Medicaid ID, date of birth, provider name and signature, certification date, a specific statement of medical necessity, and the type of transportation required (e.g., wheelchair van or stretcher). A 2023 DHCS audit revealed that over 30% of NEMT claim denials in California stemmed from missing or incomplete PCS forms. Common issues include unsigned forms, outdated information, incomplete patient details, and vague medical necessity statements that fail to justify the transportation type.
To avoid these pitfalls, the medical necessity section must be detailed. Generic phrases like "patient needs transportation" are not enough. Providers should clearly document the patient’s medical conditions, mobility challenges, or treatment needs that make professional medical transportation essential. Once the information is verified, organizing these forms systematically becomes equally important.
PCS forms should be updated annually or whenever a patient’s medical condition or transportation needs change significantly. Setting up an automated renewal reminder system can help ensure that documentation stays current, reducing the risk of compliance issues.
Conducting regular internal audits to review PCS forms can catch errors before external auditors do. For example, in 2023, Rhode Island’s NEMT program introduced quarterly quality review sessions that included random PCS form audits. This initiative led to a 22% drop in claim denials due to documentation errors within just six months.
Being audit-ready involves more than just accurate documentation. Federal Medicaid regulations, along with state-specific guidelines, require PCS forms to justify NEMT services. These forms should be retained for 5–7 years, depending on state laws, and updated regularly to meet state-specific requirements. Failure to comply can result in denied claims, repayment demands, or even legal consequences.
State requirements vary, adding another layer of complexity. Some states mandate periodic renewal or re-certification, while others require more detailed patient information. For instance, Oregon has recently tightened its PCS documentation rules, requiring more comprehensive patient details and frequent updates to certification status.
Additionally, HIPAA compliance is a critical factor. Mishandling PCS forms can lead to fines as high as $1.5 million annually. To avoid this, organizations must prioritize secure storage, controlled access, and proper disposal as part of their compliance strategy.
Trip documentation records serve as proof that every Non-Emergency Medical Transportation (NEMT) ride meets billing and regulatory standards. Auditors rely on these records to confirm that services were delivered as claimed, ensuring there’s no fraud while verifying that the transportation provided was medically necessary and properly authorized. This documentation not only safeguards patient safety but also ensures smoother audit processes by providing clear, verified evidence.
These records are especially important when auditors compare them with dispatch logs, billing records, and GPS data. Any inconsistencies can lead to deeper investigations, claim denials, or even financial penalties.
Auditors closely examine trip records for accuracy, consistency, and legibility. Common mistakes that can raise red flags during audits include missing or unreadable signatures, incomplete trip details (such as omitted pickup or drop-off times), mismatches between trip logs and billing records, and failure to document no-shows or cancellations properly. Errors like incorrect mileage reporting or missing documentation to support medical necessity are also frequently flagged.
Ensuring that documentation is completed in real time helps maintain authenticity and reduces the chances of errors or omissions.
Once the records are accurate, keeping them well-organized is key to simplifying audit reviews. Digital documentation systems have proven far more efficient than paper-based methods. For example, in 2024, the Oregon Health Authority required NEMT providers to submit detailed trip logs and patient data records for Coordinated Care Organizations (CCOs). Providers using digital systems in Oregon saw a 25% drop in claim denials. Regular internal audits also help minimize discrepancies.
"Bambi has been able to kind of streamline that whole process...it just takes me half the time, or probably even less than that, to get everything kind of squared away."
– Samuel Harris, On Time On Target Transportation
Modern software solutions offer automated GPS-based trip logs, ensuring accurate, timestamped records - even in areas with poor connectivity. These systems can capture offline GPS-stamped events, providing a complete picture and enabling providers to address potential issues before they escalate.
Providers must retain trip records for at least six years to meet federal and state audit standards. Some states or payers may require even longer retention periods, so it’s essential to confirm specific requirements. Records must also be safeguarded against loss, tampering, or unauthorized access. Failure to maintain proper documentation can result in serious consequences, including claim denials, payment recovery demands, financial penalties, suspension or termination from Medicaid programs, and damage to a provider’s reputation. In severe cases, providers could face legal action or even lose their licensure.
States are increasingly requiring detailed trip logs and comprehensive patient data, reflecting a broader push for transparency and accountability in NEMT operations. Regular staff training on documentation standards and updates to coding practices can further reduce errors and enhance compliance. These efforts not only support audit readiness but also align with the broader goal of maintaining high standards across NEMT services.
After patient and trip records, vehicle compliance documents are another critical piece of the puzzle when it comes to demonstrating operational safety. These records confirm that your fleet meets the safety standards set by federal, state, and Medicaid guidelines - an essential requirement for Non-Emergency Medical Transportation (NEMT) providers. Auditors closely examine these documents to ensure every vehicle in your fleet is properly registered, regularly inspected, and equipped with all mandatory safety features. Any gaps in this documentation can raise red flags.
The Department of Transportation (DOT) mandates annual inspections for all vehicles, and auditors will cross-check your fleet records against the vehicles in active service. Missing or incomplete documentation can lead to severe consequences, including compliance violations, service suspensions, or even contract termination.
To stay compliant, your vehicle files need to include several key documents: current registration, commercial auto insurance, inspection certificates, maintenance logs, and equipment checklists (like those for wheelchair securements, fire extinguishers, and first aid kits). These records must align with your active fleet.
Common issues that auditors flag include expired inspection certificates, missing insurance papers, incomplete maintenance logs, and lack of proof for safety equipment. Vehicles that aren’t properly registered or haven’t undergone required safety checks can jeopardize compliance and, more importantly, patient safety.
In 2024, the Oregon Health Authority introduced stricter NEMT compliance rules, requiring providers serving Coordinated Care Organizations (CCOs) to maintain more detailed safety logs and inspection records. Providers who failed to meet these updated standards during audits faced corrective actions, and in some cases, temporary suspension of their service contracts.
Managing vehicle compliance has become much more efficient with the use of digital record-keeping systems. For instance, a California-based provider utilized a digital platform to track inspections, insurance renewals, and maintenance logs. This system allowed them to instantly pull up accurate and up-to-date records during a Medicaid audit, ensuring a smooth review process.
| Inspection Type | Frequency | Documentation Required | Retention Period |
|---|---|---|---|
| Comprehensive Safety Check | Annual | Full inspection report | 3 years |
| Post-Repair Inspection | After major repairs | Repair documentation & safety verification | 3 years |
| Routine Maintenance | Quarterly | Service records & maintenance logs | 3 years |
DOT guidelines require that vehicle inspection records be kept for at least three years, though some states may demand longer retention periods. To stay audit-ready, it's crucial to review and update records quarterly, especially after inspections, maintenance work, or regulatory changes. Conducting internal audits before external ones can help catch and fix any gaps early.
For example, Rhode Island’s NEMT program conducts bi-monthly oversight meetings and quarterly quality review sessions, which include spot checks of vehicle compliance and inspection records. Providers who consistently maintain accurate and complete documentation have avoided penalties and ensured uninterrupted Medicaid contracts. Across the board, states are emphasizing real-time documentation and more detailed compliance measures.
Driver credentials and training records play a critical role in passing a Non-Emergency Medical Transportation (NEMT) compliance audit. These records are often under intense scrutiny because they ensure that drivers meet the necessary federal, state, and Medicaid standards for safely transporting patients who may be vulnerable. The Non-Emergency Medical Transportation Accreditation Commission (NEMTAC) has raised the bar with its emphasis on standardized driver education and data-driven compliance, signaling a move toward stricter industry expectations.
The stakes are high. For example, violations under HIPAA due to improper training or missing documentation can lead to penalties of up to $1.5 million annually. Auditors don’t just check if the paperwork exists - they verify that drivers hold the proper credentials to handle medical transport responsibilities while safeguarding patient confidentiality. Below, we break down the specific documentation required to meet compliance standards.
Every driver’s file must demonstrate their qualifications and compliance with current standards. Essential documents typically include:
These records must not only be accurate but also kept up-to-date to avoid compliance violations. For instance, driver’s licenses need to remain valid, background checks often require annual updates, and certifications like CPR and First Aid frequently need renewal every one to two years. Missing or outdated documentation can lead to significant compliance issues. Some states, such as Rhode Island, implement regular oversight meetings and quarterly reviews to maintain documentation accuracy.
| Required Document | Validity | Retention Period | Notes |
|---|---|---|---|
| Driver's License | Must remain valid | 3+ years | Must comply with state-specific requirements |
| Background Check | Annual or as needed | 3+ years | Includes both criminal and driving history |
| Drug/Alcohol Screening | Pre-employment & random | 3+ years | Frequency varies by state |
| CPR/First Aid Certification | Annual or biannual | 3+ years | Must be current |
| PASS Certification | Annual | 3+ years | Passenger Assistance Safety & Sensitivity |
| HIPAA Training Certificate | Annual | 3+ years | Proof of privacy compliance |
Having accurate records is only part of the equation - quick and efficient access to these documents is equally important. Platforms like Bambi streamline this process by digitally storing and organizing driver files, setting automated alerts for expiring credentials, and tracking training completions. These systems can also schedule refresher courses, ensuring no deadlines are missed.
Best practices for organizing documentation include using standardized naming conventions, secure cloud-based storage for easy access and backups, and automated reminders to flag upcoming renewals. These tools significantly reduce administrative stress, minimize errors, and ensure that records are readily available during audits. Automated systems that notify you weeks in advance of impending expirations can save you from last-minute scrambling.
To comply with federal, state, and Medicaid regulations, NEMT providers must ensure their drivers meet specific criteria. This includes valid driver’s licenses, clean driving records, thorough background checks, drug testing, and certifications for key training programs like CPR, First Aid, and passenger assistance. Drivers must also complete training on HIPAA and ADA requirements to maintain patient safety and privacy. Falling short of these requirements can result in hefty fines, loss of contracts, or exclusion from Medicaid programs.
Providers are generally expected to retain driver and training documentation for at least three years, though some states or payers may require longer retention periods. To stay prepared for audits, experts suggest conducting monthly internal reviews of driver files to confirm that all credentials and training records are up to date.
Establish clear documentation policies, keep staff informed of regulatory changes, and utilize digital compliance tools to avoid potential issues. Regular internal audits can help identify and address problems early, ensuring your processes hold up under scrutiny during formal audits.

Having valid business licenses and Medicaid enrollment certificates is a must for running a legally authorized NEMT operation and billing Medicaid. These documents are among the first things auditors will ask for to confirm your compliance with state and federal regulations. If your licenses or certificates are missing or expired, you could face fines, service suspension, or even termination. Double-check that all the information on these documents is accurate and up to date to avoid unnecessary issues.
When it comes to licensing and Medicaid documentation, precision matters. Auditors expect these documents to be current and free of errors. This includes having updated state and local business licenses, NEMT provider licenses (if required), Medicaid enrollment certificates, and validated NPI/EIN documentation.
Common problems include expired licenses, mismatched business names or addresses, outdated Medicaid enrollment records, and delays in updating documents after changes in your business. Even small mistakes, like unsigned certificates, can lead to corrective actions or disqualification.
| Document Type | Typical Renewal Period | Risk Level if Missing |
|---|---|---|
| Business License | Annual/Biennial | High (service suspension) |
| Medicaid Enrollment Certificate | Varies by state | High (billing denial) |
| State NEMT Provider License | Annual | High (operational shutdown) |
| NPI Documentation | No expiration | Medium (billing complications) |
Keeping your licenses and certificates organized doesn’t have to be a hassle. A centralized digital storage system can simplify management and retrieval. Cloud-based platforms with secure, role-based access allow for quick access to documents, automated renewal reminders, and reliable backups.
For example, tools like Bambi's AI-powered compliance management system can digitize and securely store your records, send alerts for upcoming renewals, and make it easy to retrieve documents during audits. Assigning a dedicated staff member to oversee compliance tracking can further ensure everything stays in order.
Being prepared for audits means understanding that licensing and Medicaid enrollment requirements can vary by state. Some states might ask for additional permits on top of a standard business license, or require periodic revalidation of Medicaid enrollment.
To stay audit-ready, conduct regular internal reviews - monthly checks are a good practice - to ensure all documentation is accurate and complete. Automated renewal alerts can also help avoid missed deadlines. Remember, NEMT providers are typically required to keep business and Medicaid-related records for at least three years.
Failing to maintain proper documentation can lead to serious consequences, such as service suspension, contract termination, or hefty fines. In some cases, improper documentation practices could even result in HIPAA penalties of up to $1.5 million annually.
To avoid these risks, make it a habit to review and update all licenses and certificates regularly. Ensure that business names, addresses, and NPI numbers are consistent across all documents, and stay on top of any regulatory changes in your state that could impact your compliance requirements.
Preparing for an audit doesn’t have to feel overwhelming. The secret lies in having a clear, systematic approach that makes locating and presenting documents quick and straightforward. When auditors show up, you want to be able to access any record in minutes - not hours. By embracing organized digital systems, you can streamline your audit preparation process and avoid unnecessary stress.
Why digital systems are the way to go: Paper records can easily go missing, become outdated, or be incomplete, which can turn audits into a logistical nightmare. Imagine an auditor requesting all trip records from six months ago - would you rather sift through stacks of paper in filing cabinets or simply type a search query into a digital database?
More and more NEMT providers are ditching traditional filing systems, and it’s easy to see why. Digital platforms offer benefits paper simply can’t match, like secure backups, searchable archives, and automated tracking. Cloud-based systems, for instance, allow role-based access, so your compliance officer can retrieve the necessary documents while still maintaining strict security.
Digital tools also centralize critical documents. For example, digital credential wallets store driver certifications, licenses, and training records in one secure location. Instead of managing individual paper certificates, everything is digitized, and you can rely on automatic alerts for expiration dates to stay ahead of compliance deadlines.
Speaking of deadlines, automated expiry tracking tools are a game-changer. The Department of Transportation mandates annual vehicle inspections and post-repair checks. Relying on manual systems to track these dates can lead to errors, but digital platforms send reminders well in advance, reducing the risk of missed deadlines.
Another helpful feature is exception reporting, which flags missing or outdated documents before they become a problem during audits. Monthly exception reports can highlight gaps, like expired certifications or incomplete trip records, giving you time to address issues proactively.
Understanding document retention policies is another critical aspect of audit readiness. Digital systems simplify this by archiving older records automatically while still keeping them searchable and accessible. For example, the Oregon Health Authority now requires more detailed trip logs and patient data records, reflecting a trend toward stricter documentation standards. A well-organized digital system allows you to adapt to these evolving requirements seamlessly.
Security is non-negotiable, especially when dealing with sensitive information. HIPAA violations can result in fines of up to $1.5 million annually. Digital systems help you meet these standards by incorporating encryption, access controls, and audit logs - all while making document retrieval faster and easier.
One of the best ways to prepare for audits is by conducting regular internal reviews. Monthly or quarterly audits are now standard practice for many organizations, helping to identify and resolve compliance issues before external auditors step in.
Alex Stoia from Corazon Concierge shared how digital tools transformed their operations:
"Integrating advanced scheduling software and real-time tracking systems has revolutionized how we operate. Our efficiency has improved dramatically, leading to better service for our clients."
To build an effective system, choose a platform that can handle multiple compliance needs at once. Look for one that consolidates trip documentation, vehicle inspections, driver credentials, and business licenses into a single platform. This way, you’ll have all your bases covered, from trip logs to certifications.
Don’t overlook staff training - it’s just as important as the system itself. Ensure everyone who handles documents knows how to use the system effectively. Regular training sessions can prepare your team to retrieve information quickly, even in the absence of key personnel. By combining the right tools with a well-trained team, you’ll be ready for any audit that comes your way.
Switching from manual compliance methods to AI-powered platforms has revolutionized how Non-Emergency Medical Transportation (NEMT) providers handle their operations. Paper-based systems often lead to misplaced documents and costly mistakes, whereas modern tech solutions ensure everything is organized and audit-ready.
Automation plays a crucial role in keeping up with ever-changing regulations. For instance, by 2025, federal updates will require prior authorization, faster review times, and specific retention rules for critical records. Keeping track of these changes manually can be overwhelming. In contrast, AI-powered platforms automatically generate and organize the needed documentation, making audits smoother and less prone to errors.
Take Bambi's AI-powered platform as an example. It simplifies compliance by consolidating five essential audit documents into a single, searchable system. Instead of rummaging through physical files during an audit, providers can instantly access Physician Certification Statements, trip records, vehicle inspections, driver credentials, and business licenses through automated workflows. It’s a game-changer for NEMT providers.
These platforms also excel in security. With encrypted storage, access controls, and detailed audit trails logging every action - whether it’s accessing, modifying, or deleting a document - they ensure the transparency auditors demand. Real-time monitoring adds another layer of oversight, keeping compliance airtight.
Another advantage? Real-time compliance monitoring. Unlike manual systems that might let certifications expire unnoticed, AI platforms send timely alerts and automatically archive older records while keeping them accessible for future reference. This proactive approach eliminates surprises during audits.
Claim rejections, a persistent issue in the industry, are also addressed. By integrating real-time eligibility checks and payer database verification, these platforms help reduce rejection rates significantly.
For further insights, the Bambi NEMT blog shares real-world success stories and practical tips on using AI-driven solutions to stay audit-ready. These resources showcase how providers have streamlined their operations and improved compliance management with technology.
Adopting AI-powered platforms doesn’t have to be overwhelming. Providers can start with phased rollouts, digitizing key documents while maintaining their current processes during the transition.
Here’s a quick comparison of manual versus AI-driven compliance management to illustrate the benefits:
| Feature | Manual Compliance Management | AI-Powered Platforms |
|---|---|---|
| Document Storage | Paper/Excel files | Secure, cloud-based, searchable |
| Audit Preparation | Time-consuming, error-prone | Automated, real-time reports |
| Regulatory Updates | Manual tracking | Automated alerts and checklists |
| Data Security | Variable, risk of breaches | HIPAA-compliant, encrypted |
Investing in compliance technology pays off in more ways than one. Providers report streamlined operations, less administrative hassle, and greater peace of mind during audits. When the next audit comes around, you’ll have everything you need at your fingertips, supported by the efficiency and security of modern AI-powered systems.
Thorough documentation is the bedrock of success in Non-Emergency Medical Transportation (NEMT). The five key documents we’ve discussed - Physician Certification Statement forms, trip documentation records, vehicle inspection logs, driver credentials, and business licenses with Medicaid enrollment certificates - are essential for staying prepared for audits.
Lapses in documentation can have serious consequences, including claim denials, payment recoveries, or even exclusion from Medicaid programs. Missing trip logs, incomplete PCS forms, or absent driver training records make it impossible for auditors to verify medical necessity, often leading to penalties, fines, or operational disruptions.
The stakes are high. HIPAA violations alone can result in fines of up to $1.5 million annually, and documentation requirements are becoming stricter across the board. Cutting corners simply isn’t an option.
To steer clear of these risks, providers must act proactively. Regular internal audits, consistent staff training on documentation standards, and staying updated on regulatory changes are critical steps. If deficiencies are identified, it’s vital to implement a corrective action plan that addresses the issues, retrains employees, and revises policies to prevent future problems.
Finally, remember to retain driver and vehicle records for at least three years and trip records for six years to comply with regulations. This level of organization requires a systematic approach and often benefits from digital tools to ensure everything is properly managed over the long term.
Not having complete and accurate Physician Certification Statement (PCS) forms during an audit can spell trouble for your NEMT business. Missing or incorrect forms can lead to compliance violations, which might result in penalties, fines, or even the suspension of your operating license. Beyond the financial and legal risks, it can also harm your reputation with both regulators and your clients.
To steer clear of these problems, make sure PCS forms are filled out correctly, signed by the appropriate medical professionals, and securely stored for quick access during audits. This not only keeps your business compliant but also shows your dedication to delivering dependable and professional services.
To keep trip documentation audit-ready and in line with state and federal regulations, NEMT providers need to prioritize maintaining accurate, complete, and well-organized records. This includes essential documents like trip logs, driver certifications, vehicle inspection reports, and detailed patient transport information. Regularly updating these records and verifying them against compliance standards is a must.
Leveraging tools such as AI-powered software can make the process more manageable by simplifying documentation, scheduling, and compliance tracking. Additionally, providing ongoing training for staff on effective record-keeping practices and staying updated on regulatory changes are crucial steps to prevent compliance issues during audits.
To keep vehicle compliance and inspection records current, it's essential for NEMT providers to set up a consistent schedule for inspections and updating documentation. Make sure all vehicles receive routine maintenance, and maintain thorough records of inspections, repairs, and certifications in a centralized system that’s easy to access. Always verify expiration dates for licenses, insurance, and permits to ensure timely renewals.
Leveraging technology, like AI-driven tools, can make managing these records much easier. These tools can automate reminders for upcoming deadlines and help organize compliance-related documents efficiently. Taking these proactive measures can help prevent service interruptions and keep operations running smoothly.

When it comes to NEMT (Non-Emergency Medical Transportation) billing, understanding the difference between claim denials and rejections is critical for maintaining cash flow and reducing administrative headaches. Here's the key takeaway:
Key Stats:
To minimize these issues:
For NEMT providers, knowing the difference between claim denials and rejections is key to tackling billing challenges. While both stop payments from coming through, they occur at different points in the claims process and require distinct solutions. Here's a closer look at what sets them apart and how they impact operations.
Claim denials happen after a claim has gone through the payer's full review and adjudication process. Once submitted, the claim gets a number and is carefully examined. If the payer decides not to pay - often due to issues like missing authorizations, incorrect coding, or incomplete documentation (e.g., no proof of medical necessity) - the claim is denied.
When this happens, you'll receive a detailed explanation of the denial, typically through an Explanation of Benefits (EOB) for paper claims or an Electronic Remittance Advice (ERA) for electronic ones. These documents include specific codes and reasons, giving you a roadmap for next steps, such as filing an appeal.
The financial stakes with denials are high. Industry stats show that up to 20% of medical claims are denied or rejected on their first try. If an appeal fails, the costs may fall on the provider, leading to unpaid care expenses.
Claim rejections, on the other hand, occur earlier in the process - before the claim even reaches the payer's adjudication stage. These happen when errors prevent the claim from being accepted into the system, meaning no claim number is ever assigned.
Rejections are usually caused by administrative slip-ups. Common examples include missing patient details (like insurance ID numbers or birthdates), file formatting problems, or provider errors (such as an incorrect National Provider Identifier). These issues are flagged at the clearinghouse level, stopping the claim before it gets to the payer.
The good news? Rejections are often easier and quicker to fix. Since they stem from data entry mistakes or missing info, you can correct these problems and resubmit the claim. However, until you address the errors, payment will be delayed.
| Feature | Claim Denials | Claim Rejections |
|---|---|---|
| Process Stage | After processing and adjudication | Before processing begins |
| Claim Number | Yes, assigned by the payer | No, never assigned |
| Common Causes | Authorization issues, incorrect coding, missing documentation | Data entry errors, missing info, formatting issues |
| Resolution Method | Requires appeals or corrected claims | Fix errors and resubmit |
| Financial Impact | Can mean unpaid care if appeals fail | Delays payment until corrected |
| Documentation Provided | Detailed EOB/ERA with codes | Error messages, no formal EOB/ERA |
| Average Rework Cost | Around $25 per claim in admin expenses | Lower, mainly time spent on corrections |
Avoiding these issues starts with strong claim preparation. Up next, we'll dive into the typical causes behind denials and rejections.
Understanding the reasons behind claim denials and rejections is key to resolving them quickly and reducing payment delays. While both result in delays, the underlying causes are quite different. Let’s dive into the most frequent reasons for each.
One of the top reasons for denials is Missing Pre-Authorization. Many NEMT trips require pre-authorization to ensure they meet the payer’s coverage guidelines. Failing to obtain or properly document this approval often leads to claims being denied.
Another major issue is Insufficient or Incorrect Documentation. Claims are denied when documentation is incomplete or inconsistent. For example, if a trip report shows pickup times that don’t match the billing information or lacks evidence tying the transport to a medical appointment, the claim gets denied.
Invalid CPT/HCPCS Codes also cause denials. Using outdated, incorrect, or non-covered codes can result in automatic denials. For instance, billing for wheelchair transport when the patient actually walked is a common mistake. Claims are also denied if the codes don’t align with the patient’s specific insurance plan.
Patient Ineligibility is another common factor. Whether due to expired insurance, non-enrollment, or coverage exclusions, claims for ineligible patients are denied - even if the service was necessary and properly documented. This can leave providers with uncompensated care.
Industry estimates suggest that up to 65% of NEMT claim denials could be avoided with better preparation and processes. Other contributing factors include services not covered under a patient’s plan or claims exceeding policy limits. Providers must stay informed about each payer’s specific requirements to minimize these issues.
While denials often involve complex issues like authorization and documentation, rejections are usually tied to errors in the claim submission process.
Incorrect or Incomplete Provider and Patient Information is a leading cause of claim rejections. Simple data entry errors - like misspelled names, incorrect dates of birth, or invalid insurance numbers - can cause claims to be rejected immediately if they don’t match the insurer’s records.
Formatting Issues and Missing Required Fields are another common problem. Claims submitted with non-conforming file formats or missing mandatory information - such as patient demographics, authorization numbers, or referring physician details - are automatically rejected. Each payer has specific requirements, and leaving any required field empty triggers an instant rejection.
It’s estimated that 25–30% of initial claim submissions are rejected due to administrative errors. Fortunately, rejections are usually easier to fix compared to denials. They often just require correcting the data and resubmitting the claim.
The key difference lies in how these issues are resolved. Rejections are typically quick fixes involving accurate information and resubmission, while denials often require appeals, additional documentation, or addressing more complex issues like coverage and medical necessity. By tackling these problems effectively, providers can significantly reduce delays and ensure smoother claim processing.
When it comes to claim denials and rejections, the financial consequences can be just as daunting as their causes. These issues not only delay payments but also disrupt cash flow and pile on additional administrative tasks.
Claim denials directly cut into revenue - and often permanently. When a claim is denied, the provider doesn’t get paid for the services they’ve already delivered, leaving them to absorb the cost of uncompensated care. For providers working within tight margins, every denied claim represents a financial hit that can be hard to recover from unless the denial is successfully appealed. Even after an appeal, the costs associated with the process further eat into revenue.
Rejections, on the other hand, cause cash flow headaches by delaying payments until the errors are corrected and the claims are resubmitted. While they may not result in permanent revenue loss, the delays can still strain financial operations.
Administrative costs also climb with each problematic claim. Even though rejections are generally easier to resolve, they still require staff to identify and fix errors before resubmitting. Over time, these repetitive tasks inflate operational expenses and may even necessitate hiring additional staff. This creates a ripple effect, disrupting the overall workflow and adding financial pressure.
Denials and rejections disrupt claims management by introducing extra steps that slow down reimbursements and divert staff from their regular duties. Instead of focusing on processing new claims, billing teams must investigate the reasons for denials or rejections and address submission errors.
The level of disruption depends on the type of issue. Rejections usually cause short-term delays because they can often be resolved quickly. However, if rejections occur frequently or in large volumes, they can overwhelm billing departments, leading to significant backlogs.
Denials, however, are more complex to handle. Resolving them often requires extensive back-and-forth with payers, reviewing records, gathering additional documentation, and navigating formal appeals. This process can tie up resources for extended periods, creating long-term challenges for workflow efficiency.
Tracking these issues adds another layer of complexity. Denied claims are assigned claim numbers and can be monitored through standard channels. Rejected claims, however, never make it into the payer’s system, requiring separate tracking methods.
Technology can help ease these workflow disruptions. Tools like AI-powered platforms, such as Bambi, simplify claims management by automating error detection, ensuring all documentation is complete, and flagging potential problems before submission. By addressing issues early, these solutions minimize disruptions and free up staff to focus on core tasks that drive revenue.
When billing processes run smoothly, providers can allocate more resources to critical areas like patient care, fleet management, and business growth. Addressing these operational challenges is key to maintaining efficiency and financial stability.
Catching errors early can protect revenue and keep operations running smoothly. By combining preventive measures with effective resolution strategies, NEMT providers can address claim issues proactively and efficiently.
Keeping staff well-trained on payer requirements, coding standards, and common mistakes is a solid foundation for claims management.
Verify patient eligibility in real-time. Checking coverage and benefits before providing service ensures trips are covered under the patient’s plan. This simple step prevents denials due to ineligible services or expired coverage, saving providers from unpaid claims.
Use automated claim scrubbing tools. These tools flag errors like missing documentation, incorrect dates, or formatting issues before submission. Fixing these mistakes early avoids unnecessary rejections and keeps the claims process on track.
Conduct regular internal audits. Routine reviews of claims help identify recurring issues and systemic problems. For instance, if audits show frequent documentation errors, targeted training for staff can address the root cause.
While prevention is key, having a plan for resolving issues when they arise is equally important.
For rejected claims, correcting errors and resubmitting promptly minimizes payment delays. Keeping a log of common rejection reasons helps staff quickly identify and resolve similar issues in the future.
Handling denied claims requires a more thorough approach. Start by reviewing the payer’s explanation of benefits (EOB) to understand the reason for denial. Then, gather supporting documentation - such as physician orders, trip logs, and medical records - that proves the necessity and delivery of the service.
When submitting appeals, include a clear cover letter addressing the denial reasons and ensure it’s submitted within the payer’s deadline. Tracking appeal outcomes can reveal patterns and help refine future claims processes.
Implement tracking systems for denials and rejections. Categorizing and analyzing recurring issues allows providers to spot trends, such as frequent denials from a specific payer for insufficient documentation. This insight enables staff to prepare the required evidence upfront, reducing future denials.
Technology can play a significant role in streamlining these processes.
AI-powered claim management software automates manual tasks, reducing errors. Features like automated reminders, HIPAA compliance tracking, and real-time error detection catch problems before submission, saving time and effort.
Advanced billing software with AI capabilities can identify missing fields or inconsistencies, reducing the need for rework. Platforms featured on the Bambi NEMT blog, for example, offer tools for dispatching, scheduling, and claims management, all while ensuring compliance.
Technology delivers measurable results. In 2023, a mid-sized NEMT provider in Texas lowered their claim denial rate from 18% to 7% within six months by implementing AI-powered claim scrubbing tools and conducting monthly staff training. This effort recovered $120,000 in revenue and cut administrative processing time by 30%.
Digital documentation systems simplify claim submission. These systems automatically store and organize physician orders, trip reports, and medical records, ensuring all required paperwork is complete and readily available. This reduces the risk of denials due to missing or incomplete documentation.
NEMT claim rejections typically arise from data errors early in the submission process, while denials are tied to coverage issues identified after adjudication. Both can have a direct and often negative impact on your revenue.
The financial implications are hard to ignore. Up to 20% of claims are either rejected or denied initially, and with 65% of denials never being resubmitted, providers operating on tight budgets face significant revenue losses.
To tackle these issues head-on, consider adopting proactive measures and leveraging modern technology. Real-time eligibility checks, automated claim scrubbing tools, and consistent staff training can help catch errors before they disrupt your cash flow. Advanced, AI-powered software can also identify formatting mistakes, flag missing documentation, and ensure HIPAA compliance automatically, saving time and reducing manual errors.
Analyzing patterns in denials and rejections can uncover recurring problems. Addressing these root causes with targeted training or process adjustments ensures you're fixing the underlying issues - not just the symptoms. By doing so, you can protect your revenue and strengthen your operations.
To reduce claim denials and rejections, non-emergency medical transportation (NEMT) providers should prioritize accuracy and adherence to regulations in their operations. Leveraging AI-driven tools can simplify tasks like scheduling, dispatching, and communication, while also ensuring that all required documentation and compliance standards are properly handled.
By integrating effective technology solutions, providers can cut down on mistakes, save time, and improve service quality. This approach not only helps minimize claim-related problems but also supports more seamless day-to-day operations.
To reduce revenue loss from denied claims, NEMT providers should start by pinpointing the exact reason for the denial. This can be done by carefully reviewing the Explanation of Benefits (EOB) or the denial code issued by the payer. Common culprits include incomplete documentation, incorrect billing codes, or missing prior authorizations. Tackling these problems quickly helps avoid further delays in resubmitting claims.
It’s also essential to establish a structured system for tracking and managing claims. This involves keeping detailed and accurate records, verifying patient eligibility prior to providing services, and performing regular audits to catch potential errors early. Using technology, like AI-powered tools, can make this process more efficient, enhancing accuracy and minimizing the chances of future claim denials.
For more actionable tips on refining your NEMT operations, check out the Bambi NEMT blog. It offers practical guidance designed for providers, including advice on boosting compliance and operational efficiency.
AI-powered tools make managing NEMT claims much easier by automating repetitive tasks and cutting down on errors. For instance, they can handle scheduling and dispatching with precision, ensuring trips are assigned efficiently while reducing the need for manual intervention.
Take tools like Bambi, for example. By leveraging advanced AI, Bambi suggests optimal routes, enhances communication, and ensures compliance with industry regulations. This not only saves time and lowers costs but also allows providers to concentrate on delivering top-notch service.